A Population Health Framework for Setting National and State Health Goals David A. Kindig, MD, PhD Yukiko Asada, PhD Bridget Booske, PhD
A Population Health Framework for Setting National and State Health Goals David A. Kindig, MD, PhD Yukiko Asada, PhD Bridget Booske, PhD.
COMMENTARIES
A Population Health Framework for Setting National and State Health Goals David A. Kindig, MD, PhD Yukiko Asada, PhD Bridget Booske, PhD
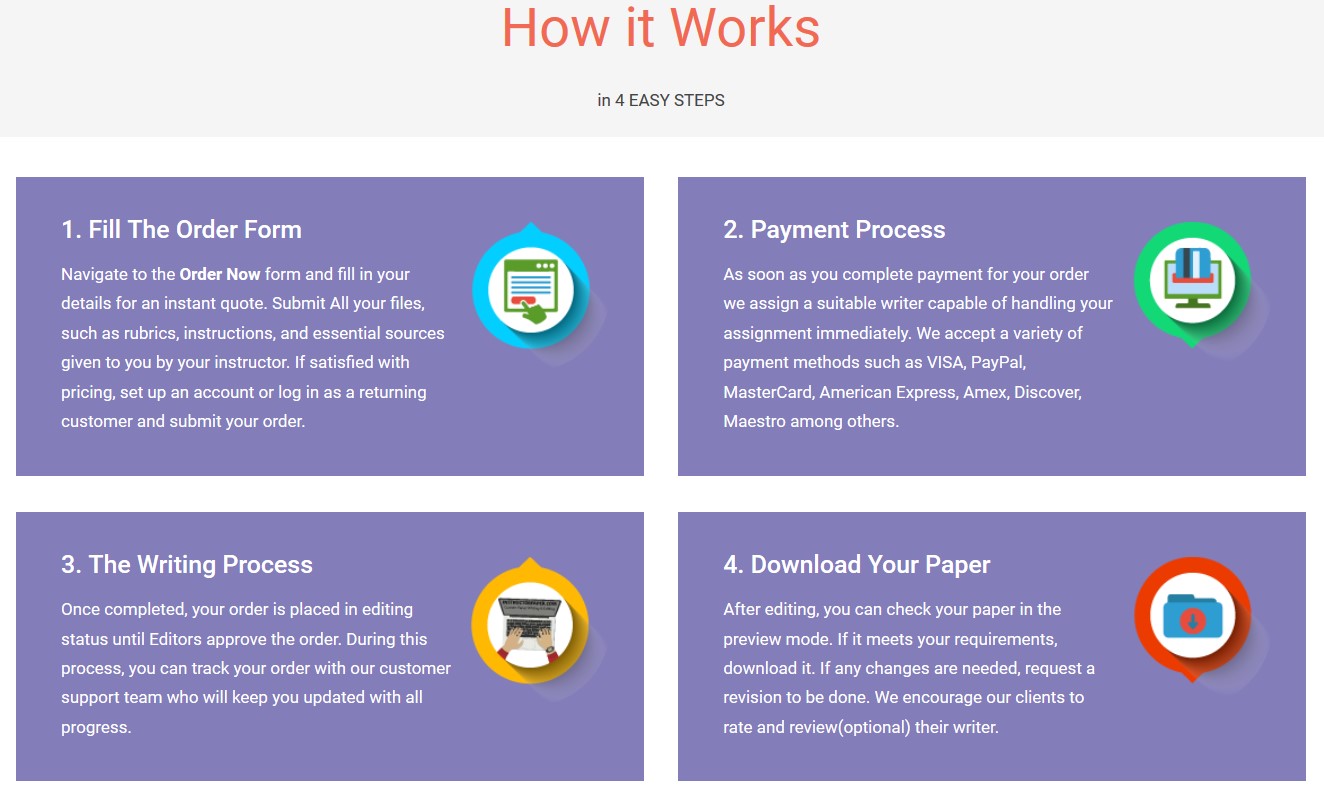
Save your time - order a paper!
Get your paper written from scratch within the tight deadline. Our service is a reliable solution to all your troubles. Place an order on any task and we will take care of it. You won’t have to worry about the quality and deadlines
Order Paper NowWITH THE APPOINTMENT OF THE US DEPART-ment of Health and Human Services AdvisoryCommittee on National Health Promotion andDisease Prevention for 2020, the process for set- ting national health goals in 2009 for the coming decade is under way. The Healthy People 2010 goals and objectives have served as the framework for establishing outcomes for virtu- ally every public health planning process in the United States from National Institutes of Health grants to federal health pro- grams and to state and local health plans. Although an initial process produced a Draft Model with 4 guiding principles and a proposal for a smaller number of objectives for Healthy People 2020, a specific framework has not yet been decided and will be established after a series of public hearings.1
This Commentary proposes a population health guiding framework for national and state planning processes, in- cluding both broad overall goals as well as a prioritized set of policies and interventions aligned with the multiple de- terminants of health.
The ultimate purpose of population health policy is to im- prove the health of individuals and populations by invest- ments in the determinants of health through policies and interventions that influence these determinants.2 Without careful attention to the outcomes, attention to determi- nants and policies could proceed without reference to the ultimate goals and become ends instead of means to an end. A shortcoming of this step of broader goal setting is that it is often framed in general terms without quantification, so it is not likely that the impact of making progress on some objectives can be assessed. Healthy People 20103 devoted significant attention to the 467 objectives in 28 focus areas, but the 2 broad goals of “increasing quality and years of healthy life” and “eliminating disparities” did not have speci- fied quantitative targets. Although the “Healthy People in Healthy Communities” model in Healthy People 2010 con- tains health determinant categories, the focus areas are pre- sented alphabetically rather than by determinant.
The FIGURE is a model that could be a starting point for a framework more precisely aligned to a population health perspective. The right side represents a way of conceptual-
izing broad population health outcomes. Previous health im- provement frameworks have identified both increasing the overall population mean, as well as reducing and eliminat- ing disparities within the population. Within disparities, mul- tiple domains could be policy targets such as race/ ethnicity, socioeconomic status, sex, and geographic location. In addition, such outcomes should include both length of life (mortality) and health-related quality of life.
Although it is possible to combine all 4 quadrants into a single summary measure, considering them separately is im- portant because different patterns of determinants will prob- ably produce different changes in each of them. Each quad- rant in the Figure is arbitrarily sized equally, and similarly the domain bars within the disparity quadrants are depicted as equal. It is probably not the case that each quadrant or do- main should receive equal weight. This is not an empirical is- suebut ratheroneof social valuation fordifferentnations, states, or other population groups to decide. The point of present- ing them this way is to encourage such consideration as a com- ponent of goal setting, which has been done occasionally. For example, the World Health Report 2000 weighted the mean and disparity equally based on a survey of about 1000 respon- dents.4 Similarly in a State Health Report Card for Wiscon- sin,5 equal weighting was primarily used, although the method used for summarizing disparities across domains resulted in slight variation from equality.
The Figure’s left-hand side represents the determinants of the population health outcomes represented on the Figure’s left side. Based on the Evans-Stoddart model,6 these deter- minants are divided into 5 categories. For example, medi- cal care includes prevention, treatment, and management of disease. Examples of individual behaviors are smoking, exercise, and eating habits. The social environment in- cludes socioeconomic factors, most often measured by in- come, educational level, and occupation, while the physi- cal environment consists of air and water quality as well as the built environment, ie, the constructed structures such as buildings, roads, parks, and other physical infrastruc- ture that make up communities. Genetics refers to inher-
Author Affiliations: School of Medicine and Public Health, Department of Popu- lation Health Sciences, University of Wisconsin, Madison (Drs Kindig and Booske) and Department of Community Health and Epidemiology, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada (Dr Asada). Corresponding Author: David A. Kindig, MD, PhD, Population Health Sciences, University of Wisconsin, 610 Walnut Room, 760 WARF, Madison, WI 53726 (dakindig@wisc.edu).
©2008 American Medical Association. All rights reserved. (Reprinted) JAMA, May 7, 2008—Vol 299, No. 17 2081
Downloaded From: by a Walden University User on 03/19/2018
ited characteristics that determine health outcomes, most of which are unmodifiable at this time although genomics holds some promise for future intervention.
Although these determinant categories are listed inde- pendently, they have substantial and complex interactions with each other over the life course. The Figure also con- tains a small arrow going from outcomes to the determi- nant categories. This is a reminder that some outcomes also have a “reverse causality” on determinants; an example is that certain social determinants, like income, have an im- pact on outcomes, yet the health outcome of being un- healthy also can have a negative effect on income.
These determinants are drawn as making equal contribu- tions to outcomes. Although this is ultimately an empirical question rather than one of social valuation, it is unlikely that the equality depicted is correct. For example, McGinnis et al7 indicated that about 40% of deaths are caused by behav- ioral factors and assigned 30% to genetics, 15% to social cir- cumstances, 10% to medical care, and 5% to physical envi- ronmental exposures. In contrast, Cutler et al8 assigned a 50% weight to medical care while including sensitivity analysis vary- ing this weight from 25% to 75%. These differences exist be- cause such cross-sectoral economic analysis is complicated by issues of interactions between determinants and the la- tency over time of their effects; Stoddart9 has called under- standing the balance of determinants the “fantasy equa- tion,” reflecting the difficulty of such analysis.
However, recognizing the complexities involved should not deter further investigation, and at the very least spe- cific policy and intervention objectives should be grouped under these or similar determinant categories. Evidence from
growing literature on multiple determinants of health and health disparities should be combined with expert opinion to rank policy and intervention objectives within determi- nant categories, as well as perhaps ranking the determi- nant categories themselves. Wherever possible, economic evaluation information should be included so that the rela- tive cost-effectiveness of a policy or intervention (such as quality-adjusted life-years gained per dollar invested) be- yond simple effectiveness is considered. It would also be use- ful to have estimates of current levels of investment in the different determinant and specific objective categories while discussing 2020 goals and objectives. Given current knowl- edge, the accuracy of such rankings will be imperfect, al- though it is equally imperfect to imply that each of the 467 objectives in Healthy People 2010 would have had equal im- pact on population health outcome goals however speci- fied.
An additional consideration involves target setting. In rank- ing processes such as those used in The World Health Re- port 200010 and America’s Health Rankings 2007,11 progress is implied by moving up in the rankings over some period. Such ranking improvement is relative to the performance of other nations or states and not articulated as specific ab- solute improvement (it is possible to improve a rank while declining if all others are decreasing more rapidly). Be- cause Healthy People 2010 is not a comparative process, no targets or goals for overall mean improvement and dispar- ity reduction outcomes were specified, although they were for many specific objectives. It is useful for such planning processes to at least consider setting 5- to 10-year targets for broad outcomes, even if only looking at past trends in
Figure. A Schematic Framework for Population Health Planning
SPECIFIC POLICIES AND INTERVENTIONS
DETERMINANTS
Medical care
Individual behavior
Social environment
Physical environment
Genetics
POPULATION HEALTH OUTCOMES
Population mean health-related QOL
Population mean mortality
Mortality disparities
Race/ethnicity
Socioeconomic status
Sex
Geographic location
Race/ethnicity
Socioeconomic status
Sex
Geographic location
Health-related QOL disparities
The right side conceptualizes broad population health outcomes. The left side represents the determinants of population health outcomes. The quadrants in the out- comes component are arbitrarily sized equally, as are both the disparity domains within outcomes and the determinant categories. QOL indicates quality of life.
COMMENTARIES
2082 JAMA, May 7, 2008—Vol 299, No. 17 (Reprinted) ©2008 American Medical Association. All rights reserved.
Downloaded From: by a Walden University User on 03/19/2018
comparison to other nations or states and set a range of goals from minimal to achievable to challenging. Target setting is particularly useful when considering a balanced set of health outcomes such as those proposed herein. For ex- ample, the possibility that improving the population mean might actually increase disparities in subpopulations12 can become more apparent in such a target-setting process.
The processes used for such goal setting require care if the results are to become useful in guiding policy makers at all levels and in the public and private sectors. Although experts play an important role in supplying data and evi- dence where it exists, policy makers at all levels need to be actively involved, particularly when value choices are re- quired.13 There is no right answer to the relative impor- tance of the outcome cells in the Figure, and full discus- sions are likely to produce different estimates in different settings for different populations. But only with such com- bination of top-down and bottom-up approaches will such goals and objectives be owned by the populations in ques- tion and serve as active guidance for multisectoral invest- ment choices in an era of limited resources.14
Only once in a decade does the United States invest sig- nificant time and energy in seriously thinking about health goals and objectives for the nation. Every decade the Healthy People process has changed and matured. Incorporating pri- ority setting tied to investment choices could make the pro- cess much more useful to policy makers in the coming de- cades as they try to make the most cost-effective decisions from a modern population health perspective. Financial Disclosures: None of the authors have specific financial interests, rela- tionships, or affiliations relevant to the subject of this Commentary. Funding/Support: This Commentary was supported in part by the Robert Wood Johnson Health and Society Scholars program at the University of Wisconsin School
of Medicine and Public Health, as well as the Wisconsin Partnership Program “Mak- ing Wisconsin the Healthiest State” project. Role of the Sponsor: The funding organizations had no role in the preparation, review, or approval of the manuscript. Additional Contributions: We thank Patrick Remington, MD, MPH, for his help- ful comments, Carol Dizack, BS, for her graphic assistance, and Judy Knutson for her editorial assistance. All those acknowledged are affiliated with the University of Wisconsin School of Medicine and Public Health. They all receive compensa- tion for their work as full-time employees of the institution.
REFERENCES
1. US Department of Health and Human Services. Healthy People 2020 regional meetings Web page. http://www.healthypeople.gov/hp2020/regional/default .asp. Accessed March 31, 2008. 2. Kindig DA. Understanding population health terminology. Milbank Q. 2007; 85(1):139-161. 3. US Department of Health and Human Services. Healthy People 2020: a sys- tematic approach to health improvement Web page. http://www.healthypeople .gov/Document/html/uih/uih_bw/uih_2.htm#. Accessed March 31, 2008. . 4. Gakidou EE, Murray CJL, Frenk J. Measuring preferences on health system per- formance assessment: Global Programme on Evidence for Health Policy discus- sion paper. Geneva, Switzerland: World Health Organization; 2000:20, 1-24. http: //www.who.int/healthinfo/paper20.pdf. Accessed March 31, 2008. 5. University of Wisconsin Population Health Institute. Health of Wisconsin Re- port Card 2007. http://www.pophealth.wisc.edu/uwphi/research/report_card_2007 /report_card_2007.PDF. Accessed April 1, 2008. 6. Evans RG, Stoddart GL. Consuming health care, producing health care. Soc Sci Med. 1990;33(12):1347-1363. 7. McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002;21(2):78-93. 8. Cutler DM, Rosen AB, Vijan Sanjeep V. The value of medical spending in the United States, 1960–2000. N Engl J Med. 2006;355(9):920-927. 9. Stoddart G. The Challenge of Producing Health in Modern Economies. Toronto, ON: Canadian Institute of Advanced Research; 1995. Working Paper 46. 10. The World Health Report 2000: Health Systems: Improving Performance. Geneva, Switzerland: World Health Organization; 2000. 11. United Health Foundation. America’s Health Rankings: A Call to Action for People and Their Communities. Minnetonka, MN; 2007. 12. Graham H. Social determinants and their unequal distribution: clarifying policy understandings. Milbank Q. 2004;82(1):101-124. 13. Fox DM. The determinants of policy for population health. Health Econ Policy Law. 2006;1:395-407. 14. Kindig D. A pay-for-population health performance system. JAMA. 2006; 296(21):2611-2613.
A Clinical Blueprint to Accelerate the Elimination of Tobacco Use Michael C. Fiore, MD, MPH Carlos Roberto Jaén, MD, PhD
ON MAY 7, 2008, THE US PUBLIC HEALTH SER-vice (PHS) released the Clinical Practice Guide-line Treating Tobacco Use and Dependence: 2008Update.1 This guideline describes how clini- cians and health care systems can significantly reduce to- bacco use prevalence by delivering evidence-based treat- ments to their patients who smoke.
The story of tobacco control efforts over the last half- century is one of remarkable progress and promise. In 1965, current smokers outnumbered former smokers 3 to 1. Dur- ing the past 40 years, the rate of quitting has so outstripped
the rate of initiation that, today, there are more former smok- ers than current smokers.2 Since tobacco use rates peaked in the 1960s, smoking prevalence among adults has decreased by half, to about 20% today.2 Moreover, 40 years ago smok- ing was viewed as a habit rather than as a chronic disease, and smokers had no access to scientifically validated treatments.
Today numerous effective treatments exist and progress in the war against tobacco is accelerating. For instance, re- markable advances have been made in the scant dozen years
Author Affiliations: Center for Tobacco Research and Intervention, University of Wisconsin, Madison (Dr Fiore); and Department of Family & Community Medi- cine, University of Texas Health Sciences Center at San Antonio (Dr Jaén). Corresponding Author: Michael C. Fiore, MD, MPH, Center for Tobacco Re- search and Intervention, 1300 University Ave, Madison, WI 53706 (mcf@ctri .medicine.wisc.edu).
COMMENTARIES
©2008 American Medical Association. All rights reserved. (Reprinted) JAMA, May 7, 2008—Vol 299, No. 17 2083
Downloaded From: by a Walden University User on 03/19/2018
The post A Population Health Framework for Setting National and State Health Goals David A. Kindig, MD, PhD Yukiko Asada, PhD Bridget Booske, PhD appeared first on Infinite Essays.
"If this is not the paper you were searching for, you can order your 100% plagiarism free, professional written paper now!"