An observational study on the open-system endotracheal suctioning
An observational study on the open-system endotracheal suctioning.
CLINICAL NURSING PROCEDURES
An observational study on the open-system endotracheal suctioning
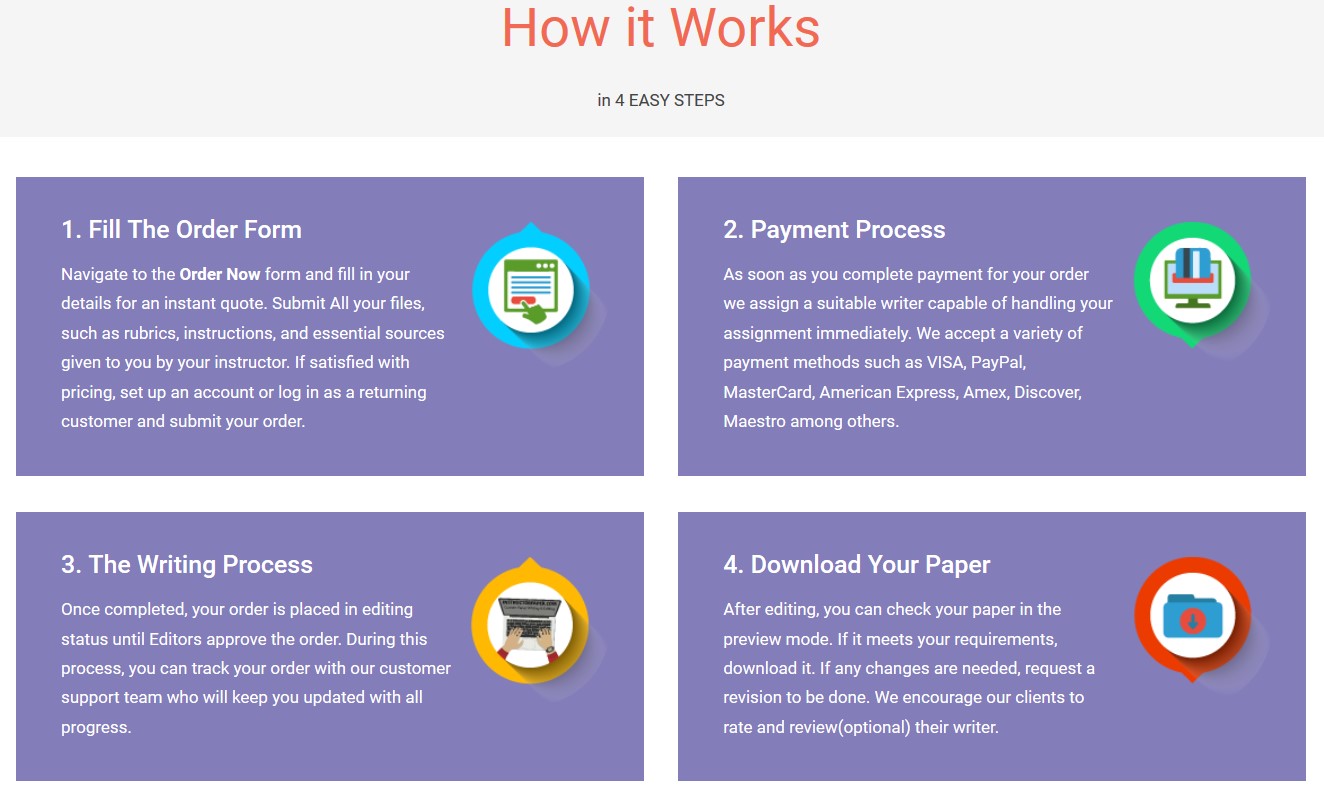
Save your time - order a paper!
Get your paper written from scratch within the tight deadline. Our service is a reliable solution to all your troubles. Place an order on any task and we will take care of it. You won’t have to worry about the quality and deadlines
Order Paper Nowpractices of critical care nurses
Sean Kelleher MSc, PGDipN (Crit. care), RGN
Lecturer, Catherine McAuley School of Nursing & Midwifery, Brookfield Health Sciences Complex, University College Cork,
Ireland
Tom Andrews PhD, PGDE, RN
Lecturer, Catherine McAuley School of Nursing & Midwifery, Brookfield Health Sciences Complex, University College Cork,
Ireland
Submitted for publication: 11 January 2006
Accepted for publication: 20 December 2006
Correspondence:
Sean Kelleher
Brookfield Health Sciences Complex UCC
Cork
Ireland
Telephone: 00353 21 4901477
E-mail: s.kelleher@ucc.ie
KELLEHER S & ANDREWS T (2008)KELLEHER S & ANDREWS T (2008) Journal of Clinical Nursing 17, 360–369
An observational study on the open-system endotracheal suctioning practices of
critical care nurses
Aim and objectives. The purpose of this study was to investigate open system
endotracheal suctioning (ETS) practices of critical care nurses. Specific objectives
were to examine nurses’ practices prior to, during and post-ETS and to compare
nurses’ ETS practices with current research recommendations.
Background. ETS is a potentially harmful procedure that, if performed inappro-
priately or incorrectly, might result in life-threatening complications for patients.
The literature suggests that critical care nurses vary in their suctioning practices;
however, the evidence is predominantly based on retrospective studies that fail to
address how ETS is practiced on a daily basis.
Design and method. In March 2005, a structured observational study was con-
ducted using a piloted 20-item observational schedule on two adult intensive-care
units to determine how critical care nurses (n ¼ 45) perform ETS in their daily practice and to establish whether the current best practice recommendations for ETS
are being adhered to.
Results. The findings indicate that participants varied in their ETS practices; did not
adhere to best practice suctioning recommendations; and consequently provided
lower-quality ETS treatment than expected. Significant discrepancies were observed
in the participants’ respiratory assessment techniques, hyperoxygenation and
infection control practices, patient reassurance and the level of negative pressure
used to clear secretions.
Conclusion. The findings suggest that critical care nurses do not adhere to best
practice recommendations when performing ETS. The results of this study offer
an Irish/European perspective on critical care nurses’ daily suctioning practices.
Relevance to clinical practice. As a matter of urgency, institutional policies
and guidelines, which are based on current best practice recommendations,
need to be developed and/or reviewed and teaching interventions developed
to improve nurses’ ETS practices, particularly in regard to auscultation
360 � 2008 Blackwell Publishing Ltd doi: 10.1111/j.1365-2702.2007.01990.x
skills, hyperoxygenation practices, suctioning pressures and infection control
measures.
Key words: clinical significance, critical care, evidence-based practice, nursing
practice, observation
Introduction
The ultimate goal of nursing is to provide evidence-based care
that promotes quality outcomes for patients, families, health-
care providers and the health-care system (Craig & Smyth
2002). While the literature has demonstrated that nurses are
increasingly recognizing the role research has to play within
modern health care (Hundley et al. 2000), it seems that many
established nursing practices are not underpinned by sound
evidence (Glacken & Chaney 2004). One area of nursing
practice that has caused concern is the endotracheal suction-
ing (ETS) of intubated patients (Swartz et al. 1996, Thomp-
son 2000, Sole et al. 2003). ETS is an important intervention
in caring for patients with an artificial airway (Thompson
2000) and an essential aspect of effective airway management
in the critically ill (Wood 1998b). It is an invasive, potentially
harmful procedure, which when performed inappropriately
or incorrectly can result in serious complications (Celik &
Elbas 2000, Paul Allen & Ostrow 2000). It is important,
therefore, that those carrying out such a procedure are aware
of the potential risks and practice in a manner that ensures
effectiveness and patient safety.
Literature review
While ETS is an important intervention when caring for
critically ill patients, the practice surrounding ETS can vary
widely between institutions and practitioners (Swartz et al.
1996, Sole et al. 2003) with much of that practice based on
anecdote and routine rather than research (Paul Allen &
Ostrow 2000, Thompson 2000, Day et al. 2002b). This may
partially have been influenced by a paucity of research
evidence to guide practitioners in the care of a patient with
an endotracheal tube (Thompson 2000). The last decade has
seen a steady increase in the body of literature relating to how
and when ETS should be performed (Glass & Grap 1995,
Wainwright & Gould 1996, Wood 1998b, Thompson 2000,
Day et al. 2002b, Moore 2003). Much of this evidence is in the
form of succinct literature reviews (Wood 1998b, Day et al.
2002a) and systematic reviews (Thompson 2000) enabling
practitioners quickly and easily to determine current research
recommendations irrespective of their ability to interpret the
research findings. Nonetheless, there is still some disparity in
regard to what exactly constitutes the best ETS practice
(Swartz et al. 1996) owing largely to a dearth of quality
research on ETS techniques. While Thompson (2000), in a
systematic review of the literature, isolated aspects of the ETS
procedure that are generally accepted as being the most
important, a lack of homogeneity and methodological flaws in
some of the studies (Thompson 2000) resulted in 13 non-
prescriptive recommendations for practice. Conversely, the
more conventional literature reviews (Wood 1998a, Day et al.
2002a, Moore 2003), which are generally regarded as being
less rigorous than systematic reviews (Dickson 2003), expli-
citly describe how ETS should be performed, but overlook the
quality of the evidence from which they originate. Notwith-
standing the lack of rigorous research concerning ETS
practice, it is generally accepted that the ETS techniques,
when used inappropriately or incorrectly can have deleterious
effects on patients (Wood 1998b, Celik & Elbas 2000, Paul
Allen & Ostrow 2000). It is important therefore to establish
how critical care nurses perform ETS and establish how it
compares with the current best practice recommendations.
Critical care nurses’ ETS practices
A study conducted by Swartz et al. (1996) used a quantita-
tive, descriptive design using a survey method to examine
‘national’ suctioning practices on 80 paediatric intensive-care
units (ICU) across the United States. The results indicated
that suctioning techniques among critical care nurses varied
and were based on a combination of nursing judgement and
ward routine. Paul Allen and Ostrow (2000) report similar
findings in a quantitative descriptive study which aimed to
identify the closed-system ETS practices of 241 randomly
selected critical care nurses. One hundred and twenty nurses
(50%) responded to a mailed questionnaire. The findings
indicated variations in nurses’ suctioning techniques. While
the results of both studies suggest that critical care nurses
vary in their ETS practices, the ‘ex-post facto’ focus of the
studies may not necessarily be an accurate reflection of
nurses’ daily practice. Carter (1996), cited in Cormack
and Benton (1996), suggests that the subjects’ written
responses to questionnaire items about how they carry out
a procedure may bear little resemblance to how they actually
perform it.
Clinical nursing procedures Critical care nurses’ suctioning practices
� 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369 361
Day et al. (2002b)) triangulated observation, interview and
questionnaire methods to explore nurses’ theoretical know-
ledge and practical competence in ETS. Using convenience
sampling, 28 critical care nurses were recruited from three
critical care wards in a large teaching hospital in the UK. The
results indicated that many nurses failed to demonstrate an
acceptable level of theoretical knowledge and competence in
practice and that there was no significant relationship
between nurses’ theoretical knowledge and observed practice.
Furthermore, many nurses were unaware of recommended
practice and some demonstrated potentially unsafe practice.
These findings are supported in the literature (Celik & Elbas
2000) and have considerable implications for the safety of
critically ill patients.
The observational element of Day et al’s. (2002a) study
ensures a more accurate reflection of what happens in
practice than the descriptive retrospective studies discussed
earlier (Swartz et al. 1996, Paul Allen & Ostrow 2000). This
view is supported in the literature, which suggests that
observational methods provide data on the realities of current
practice from a first-hand perspective (Zeitz 2005). Day
et al’s. (2002b) findings are, therefore, very significant as they
support previous research that identified wide variations in
nurses’ ETS practices (Swartz et al. 1996, Paul Allen &
Ostrow 2000) and that nurses are inclined to rely on personal
experience and ward routine to inform practice over any
other source (Sole et al. 2003).
Summary of the literature
The literature search identified a paucity of empirical
evidence relating to how well ETS is performed in the clinical
area. The literature that does exist raises concerns about the
standard of ETS practice among nurses (Paul Allen & Ostrow
2000, Day et al. 2002b). This evidence is predominantly
American and based on descriptive, retrospective studies that
focus on closed suctioning systems (Swartz et al. 1996, Paul
Allen & Ostrow 2000, Sole et al. 2003). While such studies
are important for describing and documenting the aspects of
ETS practice, they have one primary limitation. Participants
may have a tendency to misrepresent attitudes or traits by
giving answers that are consistent with prevailing social views
(Polit et al. 2001). A few observational studies addressing
nurses’ ETS practices are identifiable in the literature (Day
et al. 2002b, McKillop 2004), with only one assessing how
actual nursing practice are compared with the recommended
practice (Day et al. 2002b).
The inconclusive literature relating to nurses’ real ETS
practices indicates the urgent need for more observational
studies in this area. It is only by distinguishing between the
real and perceived ETS practice that the degree of deviance, if
any, from what the literature has established as being general
best practice, can accurately be established.
Method
Aims
The purpose of the study was to investigate open-system ETS
practices of critical care nurses. Specific objectives were to:
1 Examine critical care nurses’ practices prior to, during and
post ETS;
2 Compare nurses’ ETS practices with current research rec-
ommendations.
Based on the evidence, it is hypothesized that critical care
nurses do not adhere to the best practice recommendations
when performing ETS.
Design
A non-participant structured observational design was used
for this study to gain insight into what is happening in
practice. Structured observational studies involve the collec-
tion of data that specify the behaviours or events selected for
observation and are conducted in the participants’ natural
environments (Polit et al. 2001). Fitzpatrick et al. (1994)
suggest that direct observation is potentially a more compre-
hensive method to ascertain how nurses perform in real
situations and to identify differences, if any, in practice.
Sample and setting
The study took place in March 2005 on two adult ICU in
Ireland. At the time of the study, the general ICU (GICU) had
nine beds with the facility to ventilate patients in all beds at
any one time. The cardiac ICU (CICU) had six beds and could
facilitate the mechanical ventilation of six patients. GICU
employed 53 full-time equivalent nurses and CICU employed
34. The nurses were generally allocated to only one patient
per shift. The targeted population of interest were critical-
care nurses, as they predominantly perform ETS, while the
sampling unit was the ETS event itself. Event sampling was
deemed the most appropriate method of observation because
of the erratic nature of the ETS procedure. By means of quota
sampling, a total of 45 individual ETS events was observed,
whereby each nurse performed only one event. Quota
sampling is procedurally similar to convenience sampling;
however, the researcher can guide the selection of subjects so
that the sample includes an appropriate number of cases from
each stratum (Polit et al. 2001), the strata in this instance
S Kelleher and T Andrews
362 � 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369
being GITU nurses and CICU nurses. The sample size
(n ¼ 45) (51%) to be a representative sample of a combined total of 87 nurses (GITU 53, CITU 34) working on both ICUs
and compares favourably with previous observational studies
addressing ETS, wherein sample sizes ranged from n ¼ 9 (Blackwood 1998) to n ¼ 28 (Day et al. 2002b) observations. Inclusion and exclusion criteria were maintained.
Inclusion criteria
• Full-time ICU staff members; • Nurses with a minimum of one-year ICU experience on the
study ICU.
Participants were required to fulfil these inclusion criteria
to be considered eligible for the study. This can be justified
by the argument that an experienced ICU nurse from a
different ICU, who has recently been appointed, may work
from a different practice/knowledge base depending on the
ICU he/she comes from. Equally, nurses who have minimal
ICU experience may not have acquired/developed a satis-
factory practice/knowledge base from which to work.
Data collection
Data were collected using a 20-item structured observational
schedule (Appendix) adapted from a previously validated
survey tool (McKillop 2004), which was constructed to
reflect the observable behaviours associated with best-prac-
tice suctioning of adults with an artificial airway (Thompson
2000). Aspects of ETS practice that were not specified in the
observational schedule developed by McKillop (2004) but
implied in a systematic review by Thompson (2000) and
established elsewhere as best-practice recommendations (Day
et al. 2002a, Wood 1998a) were added to the instrument on
the recommendation of experts in critical care nursing. The
observational schedule was piloted to identify practical or
local problems that might potentially affect the research
process. No changes were made to the instrument based on
the pilot study.
All items on the observational schedule were weighted with
the digits 0 and 1, or 0 and 2, respectively. The higher
weighting (2) constituted adherence to the best ETS practice
as recommended by Thompson (2000) following a systematic
review of the literature. The lower weighting (1) represented
adherence to what is marginally accepted as constituting best
ETS practice as they emanate from traditional literature
reviews (Day et al. 2002a, Moore 2003). The weighting of 0
represented non-adherence to either of the aforementioned.
High observation scores represented closer adherence to
recommended best practice.
Validity and reliability
The observational schedule was distributed for appraisal to a
range of experts in critical care nursing, including a university
lecturer in critical care nursing, two senior nursing intensive
care practitioners and the researcher who developed the
original instrument. During the pilot study, the observational
schedule was tested for interrater reliability using a second
observer, and no significant discrepancies were identified.
Ethical considerations
Ethical approval to conduct the study was obtained from the
appropriate ethics committee, and all participants were
informed that their participation was voluntary and that
their right to withdraw from the study would be respected at
all times. Measures to ensure confidentiality and anonymity
were implemented.
Data analysis
Descriptive statistics included frequency ratings and percent-
ages for nominal-level data. A one-sample t-test was used to
test the null hypothesis and compare participants’ ETS
practices to ideal ETS best-practice recommendations.
Analysis was performed using the Statistical Package for
the Social Scientists (SPSS, version 9.0) software.
Quality of treatment
To assess how individual participants’ performances and
subsequently a group’s performance compared with recom-
mended best practice, a variable representing ‘recommended
best practice’ had to be developed. This was developed by
calculating the sum of the highest possible scores for each
observation, which was established as being 35. Each of the
20 items on the schedule was weighted with 0 and 1, or 0 and
2 depending on the strength of supporting evidence for that
particular aspect of ETS. The number 35 therefore represen-
ted perfect adherence to best-practice recommendations, or
ideal treatment. The higher a participant’s/group’s observa-
tional score, the closer the participant/group adhered to
best-practice recommendations. Similarly, the lower a parti-
cipant’s/group’s score, the less likely was the adherence to
best-practice recommendations. This additional variable was
subsequently termed ‘quality of treatment’. For analysis, the
variable was further divided into four subscales to describe
the different aspects of the quality of treatment: practices
prior to suctioning, infection control practices, the suctioning
event and postsuctioning practices.
Clinical nursing procedures Critical care nurses’ suctioning practices
� 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369 363
Results
In accordance with the observational schedule, the results
were divided into five sections: practices prior to suctioning,
infection control practices, the suctioning event, postsuction-
ing practices and quality of treatment.
Practices prior to suctioning
When assessing the need for ETS, only two (12%) CICU and
four (14%) GICU participants auscultated the patient’s chest
(Table 1). All CICU participants communicated in some form
to patients about the imminent procedure; however, eight
(28%) GICU participants failed to communicate in any form.
Similarly, a greater number of CICU participants were
observed to perform hyperoxygenation on patients prior to
ETS (n ¼ 16, 94%) compared with the GICU group (n ¼ 22, 79%).
Infection control practices
In relation to wearing gloves and an apron during the ETS
procedure, there was no difference between the two groups as
both were fully compliant with practice recommendations
(Table 2). Disparities in practices were noted, however, in
relation to hand washing prior to the procedure, maintaining
the sterility of the suction catheter until its insertion into the
airway and wearing goggles. Only nine (31%) GICU partic-
ipants washed their hands before performing ETS in contrast
to 11 (65%) from CICU. Ten (59%) CICU and eight (29%)
GICU participants failed to maintain the sterility of the
suction catheter prior to its insertion into the patient’s
airway. Only two (12%) CICU, participants and one (3%)
GICU participant wore goggles during the ETS procedure.
The suctioning event
Both groups complied fully with best-practice recommenda-
tions in relation to suctioning time and application of
pressure; however, all participants in both groups exceeded
the recommended suctioning pressure of 80 and 150 mmHg
(Table 3). Seven (40%) of the CICU group and eight (28%)
of the GICU group selected a catheter that was larger than the
recommended size for suctioning, and six (21%) GICU
participants required more than the maximum number of
recommended suction passes.
Table 1 Practices prior to suctioning
Variable Cardiac ICU (n ¼ 17) General ICU (n ¼ 28)
Patient assessment
No 15 (88%) 24 (86%)
Yes 2 (12%) 4 (14%)
Patient preparation
No 0 8 (28%)
Yes 17 (100%) 20 (72%)
Prehyperoxygenation/hyperinflation
Not given 1 (6%) 6 (21%)
Given 16 (94%) 22 (79%)
NaCl (sodium chloride)
No 17 (100%) 28 (100%)
Yes 0 0
ICU, Intensive-care unit; n ¼ sample number.
Table 2 Infection control practices
Variable Cardiac ICU (n ¼ 17) General ICU (n ¼ 28)
Hand washing
No 6 (35%) 19 (69%)
Yes 11 (65%) 9 (31%)
Gloves wearing
No 0 0
Yes 17 (100%) 28 (100%)
Apron wearing
No 0 0
Yes 17 (100%) 17 (100%)
Catheter sterility
No 10 (59%) 8 (28%)
Yes 7 (41%) 20 (72%)
Goggles
No 14 (88%) 27 (97%)
Yes 2 (12%) 1 (3%)
ICU, Intensive-care unit; n ¼ sample number.
Table 3 The suctioning event
Variable
Cardiac ICU
(n ¼ 17) General ICU
(n ¼ 28)
Catheter size
>Half internal diameter of ETT 7 (40%) 8 (28%)
£ Half internal diameter of ETT 10 (60%) 20 (72%) Number of suctioning passes
More than two 0 6 (21%)
Two or less 17 (100%) 22 (79%)
Suction time
>15 seconds 0 0
£ 15 seconds 17 (100%) 28 (100%) Suction pressure
80–150 mmHg 0 0
>150 mmHg 17 (100%) 28 (100%)
Suction applied during
Withdrawal 17 (100%) 28 (100%)
Insertion 0 0
ETT, endotracheal tube; ICU, Intensive-care unit; n ¼ sample number.
S Kelleher and T Andrews
364 � 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369
Postsuctioning practices
Two (12%) participants from CICU and seven (24%) from
GICU failed to provide post-ETS hyperoxygenation (Table 4).
Only one (6%) CICU participant and two (7%) GICU
participants auscultated the patients’ chest to evaluate the
effectiveness of the ETS procedure. The main differences
between the groups were in relation to hand washing and
providing reassurance, with four (23%) CICU participants
failing to wash their hands after the ETS procedure in
comparison to 11 (38%) GICU participants. Patients were
reassured by 15 (88%) CICU participants in contrast to 11
(38%) from GICU.
Quality of treatment
Using a frequency distribution, the average treatment quality
across both groups was 22Æ62 (SD ¼ 3Æ10) (Table 5). The
quality of treatment scores ranged from 14–30. Within the
subscales, the highest average score was found in postsuc-
tioning practices (mean ¼ 6Æ47, SD ¼ 1Æ53) and the lowest average score was found in infection control measures
(mean ¼ 4Æ67, SD ¼ 1Æ17). A symmetric distribution was identified in the variable ‘treatment quality’ and its subscales.
Testing the null hypothesis
To compare participants’ ETS practices with best-practice
recommendations, a one-sample t-test was conducted, which
compared the treatment quality observed with the ideal
treatment quality score (Table 6). The test identified signifi-
cant differences between the quality of treatment and its
subscales (representing the combined ETS practices on both
units) and the perfect score (representing recommended best
practice). In all categories, the quality of treatment observed
was significantly lower than the quality of treatment required
(p ¼ 0Æ01). This indicates that our study’s sample group only partially adhered to best-practice recommendations when
performing ETS and hence rejects the null hypothesis.
Discussion
The findings from this study have raised some interesting
issues relating to the current ETS practice of critical care
nurses. Best-practice ETS recommendations suggest that,
when performing a respiratory assessment, nurses should
auscultate the patient’s chest to verify the need for ETS
(Thompson 2000, Day et al. 2002a, Wood 1998a). Our
findings show that the participants generally failed to do this.
Day et al. (2002b) reported similar findings in a study of
acute and high-dependency ward nurses. Their findings
showed that only two nurses were observed to have
performed auscultation. Given that the majority of partici-
pants failed to auscultate lung sounds prior to ETS, it is
possible that they were working from a combination of
clinical signs that indicated the necessity for ETS, such as
Table 4 Postsuctioning practices
Factor Cardiac ICU (n ¼ 17) General ICU (n ¼ 28)
Oxygen reconnection
>10 seconds 0 1 (3%)
<10 seconds 17 (100%) 27 (97%)
Postsuctioning hyperoxygenation
No 2 (12%) 7 (24%)
Yes 15 (88%) 21 (76%)
Post-ETS assessment
No 16 (94%) 26 (93%)
Yes 1 (6%) 2 (7%)
Patient reassured
No 2 (12%) 17 (62%)
Yes 15 (88%) 11 (38%)
Hand washing postsuctioning
No 4 (23%) 11 (38%)
Yes 13 (77%) 17 (62%)
Safety
No 0 0
Yes 17 (100%) 17 (100%)
ICU, Intensive-care unit; n ¼ sample number.
Table 5 Quality of Treatment
Practices Prior
to Suctioning
Infection Control
Practices
Suctioning Event
Practices Post Suctioning
Quality of
Treatment
N 45Æ00 45Æ00 45Æ00 45Æ00 45Æ00 Mea 5Æ56 4Æ67 5Æ93 6Æ47 22Æ62 Median 6Æ00 5Æ00 6Æ00 7Æ00 23Æ00 Mode 6Æ00 5Æ00 7Æ00 8Æ00 25Æ00 Standard Deviation (SÆD) 1Æ27 1Æ17 1Æ12 1Æ53 3Æ10 Range 6Æ00 5Æ00 5Æ00 6Æ00 16Æ00 Minimum 2Æ00 3Æ00 2Æ00 3Æ00 14Æ00 Maximum 8Æ00 8Æ00 7Æ00 9Æ00 30Æ00
Clinical nursing procedures Critical care nurses’ suctioning practices
� 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369 365
noisy breathing or visible secretions in the airway (Thompson
2000). A limitation of observational methods, however,
meant that there was no way of establishing whether
participants’ decision to perform ETS was informed by such
indicators or whether they were working from some other
perspective, such as unit routine, as is suggested in the
literature (Swartz et al. 1996, Day et al. 2002a).
Despite abundant evidence on the negative consequences of
suctioning induced hypoxemia (Wood 1998a, Thompson
2000, Day et al. 2002a) 17 participants still failed to provide
hyperoxygenation/hyperinflation either before and/or after
ETS. Day et al. (2002b)) reported similar findings, where only
two out of 10 subjects in their study were observed to provide
hyperoxygenation/hyperinflation in practice. Such findings
are important as they have direct implications for patient
safety and reflect poorly on a vital aspect of nursing care.
Nosocomial infections are among the most common
complications affecting hospitalized patients (Burke 2003).
Consequently, the importance of aseptic technique in suc-
tioning practices and hand washing before and after such
procedures is strongly emphasized in the literature (Thomp-
son 2000, Wood 1998a, Day et al. 2002a). Twenty-five
participants in our study were not observed to wash their
hands prior to the ETS procedure. Boyce and Pittet (2003)
suggest that nurses do not wash their hands as expected
because of the time it takes out of a busy work schedule,
particularly, in high-demand situations, such as critical care
units, under busy working conditions and at times of
overcrowding or understaffing. One study conducted in an
ICU demonstrated that it took nurses an average of 62 sec-
onds to leave a patient’s bedside, walk to a sink, wash their
hands and return to patient care (Boyce & Pittet 2003).
Notably, however, all participants in our study were
observed to wear gloves and an apron during ETS. This
may suggest a perception among nurses that wearing gloves
and using a ‘non-touch’ aseptic technique when inserting the
suction catheter negates the need for frequent hand washing.
However, the literature clearly suggests that gloves do not
replace the need for hand washing (Pratt et al. 2001). These
findings support earlier studies that report modest and even
low levels of adherence to recommended hand-hygiene
practices (Thompson 2000, Boyce & Pittet 2003).
Another area of particular concern is the suction pressure
used when performing ETS. High negative pressure can cause
mucosal trauma, which in turn predisposes the bronchial tree
to a higher risk of infection (Wood 1998a). Using high
negative pressures does not necessarily mean that more
secretions will be aspirated; therefore, limiting pressures to
between 80–150 mmHg is recommended (Wood 1998a,
Thompson 2000, Day et al. 2002a). The results indicated
that all participants used suction pressures outside the
recommend levels for safe practice with suction pressures
ranging form 230 to 450 mmHg. Participants on GICU
generally used lower suctioning pressures, ranging from 230–
380 mmHg, which still exceeded the recommended pressures
for safe practice. Again these findings support the study by
Day et al. (2002b) which found nurses to be generally
unaware of recommended best ETS practice.
Recommendations for education, practice and research
• As a matter of urgency, institutional policies and guide- lines, which are not based on current best-practice rec-
ommendations, need to be developed and/or reviewed.
• Teaching interventions to improve nurses’ knowledge and competence in the care of patients requiring ETS is indi-
cated particularly with regard to auscultataion skills,
hyperoxygenation practices, suctioning pressures and
infection control measures.
• The orchestration and implementation of effective educa- tional interventions to change practice may be time con-
suming. Therefore, in the interim, it is recommended that
nurses become familiar with the clinical indicators for ETS
and how to perform a simple respiratory assessment on
ventilated patients.
• Infection control guidelines need to be reinforced and monitored to ensure compliance.
• A regular audit of ETS practice is recommended to ensure that patient safety is being assured.
Table 6 A comparison between
current practice and best-practice
recommendations Variable
Maximum potential score
(representing best practice)
Mean (actual
score) SD T DF
Quality of treatment 35 22Æ62 3Æ10 �24Æ63* 44 Practices prior to suctioning 8 5Æ56 1Æ27 �12Æ90* 44 Infection control practices 9 4Æ67 1Æ17 �19Æ15* 44 The suctioning event 9 5Æ93 1Æ11 �18Æ43* 44 Postsuctioning practices 9 6Æ47 1Æ53 �11Æ10* 44
*p < 0Æ01.
S Kelleher and T Andrews
366 � 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369
This observational study was successful in achieving its
objectives; however, further observational studies need to be
conducted to substantiate the findings. Observation coupled
with a form of ‘think-aloud’ methodology may uncover the
reasons behind nurses’ decisions (in ‘think-aloud’ techniques,
subjects are questioned and asked to ‘think aloud’ in regard
to a particular aspect of their ETS practice). Such method-
ologies are recognized as a useful source of data collection in
observational studies (Yang 2003).
Limitations
Observation, like other methods has its own limitations and
ethical implications (Parahoo 1997). One of the main
problems is the effect of the ‘observer’ on the ‘observed’.
This is referred to as the Hawthorne effect and is an
important threat to the validity of observational research,
whereby participants’ knowledge of being in a study may
cause them to change their behaviour (Polit et al. 2001). In
our study, the Hawthorne effect may have resulted in
participants rehearsing ETS according to evidence-based
recommendations prior to the observations. This being the
case, it could be suggested that participants’ practice is
normally of a poorer quality than the results of our study
suggests.
Given the observational nature of the study, there were
several aspects of the ETS procedure that could not be
assessed. It was not possible to determine participants’
reasons for their practice, for example, the only observable
aspect of patient assessment was the practice of auscultation,
and even then, it was not possible to determine what
participants heard and how it was interpreted. This may
have resulted in an inaccurate interpretation of some of the
data.
The sample size was not assessed for statistical significance.
A power analysis would have established accurate sample size
requirements for the study and consequently enhanced the
representativeness of the findings (Polit et al. 2001). The
evidence used to develop the observational tool for this study
derived from what might be regarded as the best evidence
available at the time of conducting the study; however, there
is still some disparity in regard to what exactly constitutes
best practice owing to the paucity of empirical research
regarding ETS.
Finally, while the study was conducted on two different
ICUs, they were both part of one institution. The findings
therefore may not be representative of the general population
of ICU nurses and threatens the external validity of the
findings. This could have been enhanced by spreading
observations over a range of sites, in different geographical
locations.
Conclusion
This study supports the general finding in the literature that
nurses adhere only partially to best-practice recommenda-
tions in relation to ETS (Celik & Elbas 2000, Paul Allen &
Ostrow 2000, Day et al. 2002b). Under the code of
professional practice, nurses are obliged to ensure patient
safety and expected by the public and their employer to
provide high-quality, efficient, well-executed and appropriate
care of individuals (Huber 2000). By failing to adhere to what
the literature has established as best ETS practice, nurses fall
short of fulfilling any of the aforementioned expectations.
Despite an increased uptake in postregistration education
among critical care nurses and a heightened interest in the
expansion of their role, the literature indicates that they
remain poor at many of the aspects of care that might be
considered basic. Nurses need to assess and improve their
current practices continually to guarantee that evidence-
based practice recommendations are being adhered to and
patient safety is being assured. This can only be achieved
when nurses become more aware of their professional
responsibilities and receive adequate support in practice.
Acknowledgement
We would like to acknowledge the advice of a statistician Itai
Beerei, University College Cork.
Contributions
Study design: SK and manuscript preparation; SK, TA.
References
Blackwood B (1998) The practice and perception of intensive care
staff using the closed suctioning system. Journal of Advanced
Nursing 28, 1020–1029.
Boyce J & Pittet D (2003) Guideline for hand hygiene in health-
care settings. Recommendations of the Healthcare Infection
Control Practices Advisory Committee and the HICPAC/SHEA/
APIC/IDSA Hand Hygiene Task Force Morbidity and Mortality
Weekly Report. Centers for Disease Control and Prevention
51(RR16), 1–44.
Burke J (2003) Infection control – a problem for patient safety. The
New England Journal of Medicine 348, 651–656.
Celik S & Elbas N (2000) The standard of suction for patients
undergoing endotracheal intubation. Intensive and Critical
Care Nursing 16, 191–198.
Clinical nursing procedures Critical care nurses’ suctioning practices
� 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369 367
Cormack D & Benton D (1996) (ed) The Research Process in
Nursing, 3rd edn. Oxford Blackwell Science, pp. 357–372.
Craig J & Smyth R (2002) The Evidence based Practice Manual for
Nurses. Churchill Livingstone, London.
Day T, Farnell S & Wilson-Barnett J (2002a) Suctioning: a review of
current research recommendations. Intensive and Critical Care
Nursing 18, 79–89.
Day T, Farnell S, Haynes S, Wainwright S & Wilson-Barnett J
(2002b) Tracheal suctioning: an exploration of nurses’ knowledge
and competence in acute and high dependency ward areas. Journal
of Advanced Nursing 39, 35–45.
Dickson R (2003) Systematic reviews. In Achieving Evidence Based
Practice. A Handbook for Practitioners (Hamer S & Collinson G
eds). Balliere Tindall, London.
Fitzpatrick JM, While AE & Roberts JD (1994) The measurement of
nurse performance and its differentiation by course of preparation.
Journal of Advanced Nursing 20, 761–768.
Glacken M & Chaney D (2004) Perceived barriers and facilitators to
implementing research findings in the Irish practice setting. Journal
of Clinical Nursing 13, 731–740.
Glass CA & Grap MJ (1995) Ten tips for safer suctioning. American
Journal of Nursing 5, 51–53.
Huber D (2000) Leadership and Nursing Care Management, 2nd
edn. Saunders, Philadelphia.
Hundley V, Milne J, Leighton-Beck L, Graham W & Fitzmaurice A
(2000) Raising research awareness among midwives and nurses:
does it work? Journal of Advanced Nursing 31, 78–88.
McKillop A (2004) Evaluation of the implementation of a best
practice information sheet: tracheal suctioning of adults with an
artificial airway. Joanna Briggs Institute Reports 2, 293–308.
Moore T (2003) Suctioning techniques for the removal of respiratory
secretions. Nursing Standard 18, 47–53.
Parahoo K (1997) Nursing research, principles, process and issues,
Palgrave Macmillan: London.
Paul Allen J & Ostrow L (2000) Survey of nursing practices with
closed system suctioning. American Journal of Critical Care 9,
9–17.
Polit D, Beck C & Hungler B (2001) Essentials of Nursing Research.
Methods, Appraisal and Utilization, 5th edn. Lippincott, Williams
and Wilkins, Philadelphia.
Pratt RJ, Pellowe C, Loveday HP, Robinson N & Smith GW (2001)
The epic project: developing national evidence based guidelines for
preventing health care associated infections. Phase 1: guidelines for
preventing hospital acquired infections. Journal of Hospital
Infection 47, S1–S82.
Sole M, Byers J, Ludy J, Zhang Y, Banta C & Brummel K (2003) A
multisite survey of suctioning techniques and airway management
practices. American Journal of Critical Care 12, 220–232.
Swartz K, Noonan D & Edwards-Beckett J (1996) A national survey
of endotracheal suctioning techniques in the pediatric population.
Heart and Lung: The Journal of Acute and Critical Care 25,
52–60.
Thompson L (2000) Suctioning adults with an artificial airway. A
systematic review. The Joanna Briggs Institute for Evidence Based
Nursing and Midwifery. Systematic Review No. 9.
Wainwright S & Gould D (1996) Endotracheal suctioning in adults
with severe head injury: a literature review. Intensive and Critical
Care Nursing 12, 303–308.
Wood C (1998a) Can nurses safely assess the need for endotra-
cheal suction in short term ventilated patients, instead of using
routine techniques? Intensive and Critical Care Nursing 14, 170–
178.
Wood C (1998b) Endotracheal suctioning: a literature review.
Intensive and Critical Care Nursing 14, 124–136.
Yang SC (2003) Reconceptualizing think aloud methodology: refi-
ning the encoding and categorizing techniques via contextualized
perspectives. Computers in Human Behaviour 19, 95–115.Avail-
able at: http://www.elsevier.com/locate/comphumbeh (accessed 11
January 2005).
Zeitz, K. (2005) Nursing observations during the first 24 hours after
a surgical procedure: what do we do? Journal of Clinical Nursing
14, 334–343.
Appendix: observational schedule
Practices prior to suctioning
1: Patient assessment
Did the nurse auscultate the patient’s chest before ETS?
0 ¼ No 2 ¼ Yes (Wood 1998a, Thompson 2000, Day et al. 2000)
2: Patient preparation
Did the nurse explain to/communicate with the patient
about the procedure?
0 ¼ No 2 ¼ Yes (Wood 1998a, Thompson 2000, Day et al. 2000)
3: Presuctioning hyperoxygenation/ hyperinflation
0 ¼ Not given 2 ¼ Given by means of manual resuscitation bag/given by ventilator (Thompson 2000, Day et al. 2000)
4: Sodium chloride instillation
0 ¼ Yes 2 ¼ No (Wood 1998a, Thompson 2000, Day et al. 2000)
Infection control practices
5: Hands are washed prior to suctioning
0 ¼ No 2 ¼ Yes (Wood 1998b, Thompson 2000, Day et al. 2000)
6: Gloves are worn
0 ¼ No 2 ¼ Yes (Wood 1998a, Thompson 2000, Day et al. 2000)
7: Apron is worn
0 ¼ No 1 ¼ Yes (Wood 1998a, Day et al. 2000)
8: Sterility of suction catheter maintained until inserted into
airway
0 ¼ No 2 ¼ Yes (Wood 1998a, Thompson 2000, Day et al. 2000)
S Kelleher and T Andrews
368 � 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369
9: Goggles/face mask worn
0 ¼ No 2 ¼ Yes (Wood 1998a, Thompson 2000, Day et al. 2000)
The suctioning event
10: Size of suction catheter ………………… Size of ETT ………………………….. 0 ¼ >Half of the internal diameter of ETT 2 ¼ £Half of the internal diameter of ETT (Wood 1998a, Thompson 2000, Day et al. 1998)
11: Number of suction passes.……………………… 0 ¼ >2 1 ¼ <2 (Thompson 2000)
12: Length of time suction applied to airway
0 ¼ More than 15 seconds 2 ¼ Less than 15 seconds (Wood 1998a, Thompson 2000, Day et al. 2000)
13: Level of suction pressure
0 ¼ <80 mmHg/ >150 mmHg 2 ¼ 80–150 mmHg (10Æ6–20 kPa) (Thompson 2000, Day et al. 2000)
14: Position of catheter when suction applied
0 ¼ suction applied during insertion 2 ¼ suction applied during withdrawal from airway only (Thompson 2000, Day et al. 2000)
Postsuctioning practices
15: Patient reconnected to oxygen
0 ¼ >10 seconds post suctioning 1 ¼ within 10 seconds post suctioning (Day et al. 2000)
16: Postsuctioning hyperoxygenation/hyperinflation
0 ¼ Not given 2 ¼ Given by means of manual resuscitation bag/ventilator (Wood 1998a, Thompson 2000, Day et al. 2000)
17: Post-ETS assessment
Did the nurse auscultate the patient’s chest?
0 ¼ No 1 ¼ Yes (Day et al. 2000)
18: Patient reassured
0 ¼ No 1 ¼ Yes (Day et al. 2000) 19: Hands washed postsuctioning
0 ¼ No 2 ¼ Yes (Wood 1998a, Thompson 2000, Day et al. 2000)
20: Used catheter and gloves are disposed of in a manner that
prevents contamination from secretions
0 ¼ No 2 ¼ Yes (Thompson 2000)
Clinical nursing procedures Critical care nurses’ suctioning practices
� 2008 Blackwell Publishing Ltd, Journal of Clinical Nursing, 17, 360–369 369
The post An observational study on the open-system endotracheal suctioning appeared first on Infinite Essays.
An observational study on the open-system endotracheal suctioning
"If this is not the paper you were searching for, you can order your 100% plagiarism free, professional written paper now!"