Childhood obesity is a major health concern in the United States (US) with significant disparities among racial/ethnic minority subgroups1 and children with lower socioeconomic status.2 National Health and Nutrition Examina- tion Survey data from 2013-2014 indicate that the prevalence of obesity is higher and occurs at a younger age among black and Hispanic youth with
Childhood obesity is a major health concern in the United States (US) with significant disparities among racial/ethnic minority subgroups1 and children with lower socioeconomic status.2 National Health and Nutrition Examina- tion Survey data from 2013-2014 indicate that the prevalence of obesity is higher and occurs at a younger age among black and Hispanic youth with.
420
Childhood obesity is a major health concern in the United States (US) with significant disparities among racial/ethnic minority subgroups1 and children with lower socioeconomic status.2 National Health and Nutrition Examina- tion Survey data from 2013-2014 indicate that the prevalence of obesity is higher and occurs at a younger age among black and Hispanic youth with
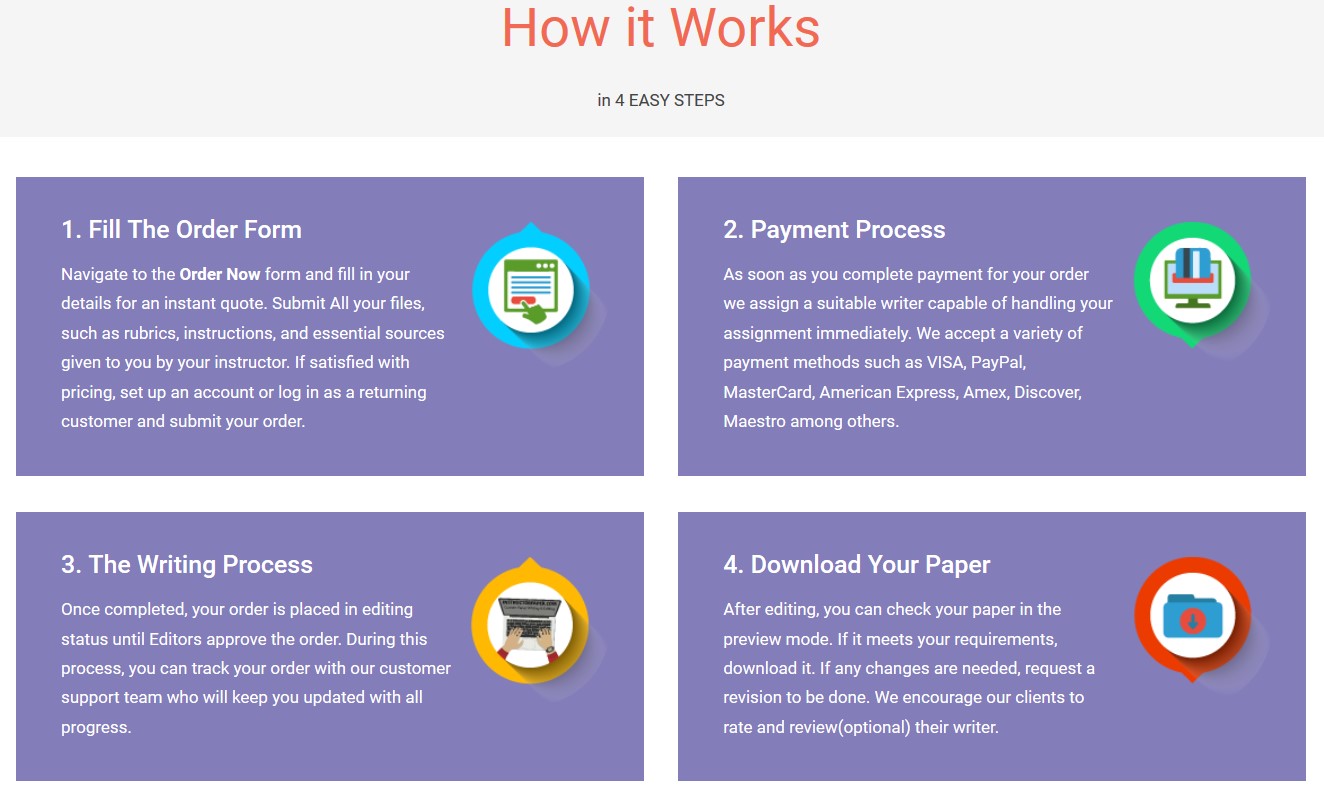
Save your time - order a paper!
Get your paper written from scratch within the tight deadline. Our service is a reliable solution to all your troubles. Place an order on any task and we will take care of it. You won’t have to worry about the quality and deadlines
Order Paper Nowthe highest prevalence (25%) found in elemen- tary school-age Hispanic youth.3 Standard of care4 to address pediatric obesity indicate that pediat- ric primary care providers (PCPs) should provide family-based counseling that includes culturally appropriate dietary and physical activity recom- mendations for behavioral change. With almost 80% of US children receiving one or more well-
Beth A. Conlon, Postgraduate Student, Albert Einstein College of Medicine, Department of Epidemiology and Population Health, Bronx, NY. Aileen P. McGinn, Associate Professor, Albert Einstein College of Medicine, Department of Epidemiology and Population Health, Bronx, NY. Carmen R. Isasi, Associate Professor, Albert Einstein College of Medicine, Department of Epidemiology and Population Health, Bronx, NY. Remaining coauthors are listed on page 434. Correspondence Dr Conlon; beth.conlon@phd.einstein.yu.edu
Home Environment Factors and Health Behaviors of Low-income, Overweight, and Obese Youth
Beth A. Conlon, PhD, RDN Aileen P. McGinn, PhD Carmen R. Isasi, MD, PhD Yasmin Mossavar-Rahmani, PhD, RDN David W. Lounsbury, PhD Mindy S. Ginsberg, BA Pamela M. Diamantis, MD Adriana E. Groisman-Perelstein, MD Judith Wylie-Rosett, EdD, RDN
Objectives: Home environment may influence children’s health behaviors associated with obe- sity. In this study, we examined home environment factors associated with diet and physical ac- tivity behaviors of overweight or obese youth. Methods: We analyzed baseline data from child and parent/caregiver dyads enrolled in an urban family weight management program. Multi- variable logistic regression examined how home environment (parenting practices, family meal habits, and home availability of fruits/vegetables, sugar-sweetened beverages (SSBs), screen media, and physical activity resources) are related to children’s intake of fruit, vegetables, and SSBs, and moderate-vigorous physical activity and sedentary time (ST) after adjusting for poten- tial confounders. Results: Children were more likely to consume fruit if their families frequent- ly ate meals together and infrequently watched TV during meals, and more likely to consume vegetables with high fruit/vegetable availability and low SSB availability. Children were more likely to engage in ST if parents practiced monitoring and frequently watched TV during meals. Conclusions: Overweight or obese children appear to have healthier habits if their families eat meals together without watching TV and if healthy food choices are available in the home. En- couraging parents to focus these practices may promote healthier body weight in children.
Key words: obesity; children; home environment; nutrition; physical activity; parenting Am J Health Behav. 2019;43(2):420-436 DOI: https://doi.org/10.5993/AJHB.43.2.17
2019;43(2):420-436 DOI: https://doi.org/10.5993/AJHB.43.2.17
Colon et al
Am J Health Behav. 2019;43(2):420-436 421 DOI: https://doi.org/10.5993/AJHB.43.2.17
2019;43(2):420-436 421 DOI: https://doi.org/10.5993/AJHB.43.2.17
child care visits annually,5 PCPs are well positioned to address parenting behaviors related to obesity. Prior research suggests that parents view PCPs as highly valued weight management advisors6,7 re- lying on the PCP to initiate weight management counsel.8 PCPs need to guide parents to become positive behavior-change agents in the prevention and treatment of childhood obesity. This includes empowering parents to create healthier home food environments and develop effective parenting prac- tices related to food and physical activity.4,9
However, there are important gaps in our under- standing of how PCPs can leverage parenting and home environment factors to promote health be- havior change,4 particularly among high risk racial/ ethnic minority populations. Limited but grow- ing evidence among Hispanic/Latino youth sug- gests that targeting parenting practices/skills and the home environment among preschool and early elementary-aged (kindergarten-2nd grade) children is effective for addressing pediatric obesity dispari- ties.10-13 However, whether parenting and home environment variables are applicable to older chil- dren, who face increased exposure to external social and environmental determinants of obesity, needs elucidation. Findings from our pediatric ambulato- ry care-based family intervention trial suggest that semi-structured PCP counseling, which includes several targets of parenting behavior, can achieve a modest improvement in body mass index (BMI) Z-scores among overweight and obese elementary school-age youth (ages 7-12 years old).14
The present study focuses on a more in-depth examination of baseline data from this cohort of predominantly Hispanic/Latino and underserved children and their parent or primary caregiver (here- after referred to as parent). The aim was to evaluate cross-sectional associations between children’s diet and physical activity behaviors and components of the home environment, including parenting prac- tices, family meal habits, home availability of fruits/ vegetables, home availability of sugar-sweetened beverages, and home availability of screen-media and physical activity resource. Results can contrib- ute to clinical practice research gaps and inform the development of primary care-based obesity preven- tion or treatment interventions that aim to target home environments of families to promote weight management, particularly among high-risk His- panic/Latino youth.
METHODS Study Design, Setting, Participants, and Procedures
The present study is a cross-sectional analysis of baseline data of the Family Weight Manage- ment (FWM) study (registered at www.clinicaltri- als.gov, NCT00851201; also known as the Fun Healthy Families Study).14 The FWM study14 was a 12-month randomized controlled trial of a pedi- atric weight management intervention conducted through a Bronx municipal hospital’s safety-net (with predominantly Medicaid coverage) primary care pediatric practice. Bronx County, New York, is a predominantly ethnic minority (53.9% His- panic/Latino; 30% non-Hispanic/Latino black or African American),15,16 low-income, urban commu- nity with an estimated childhood overweight and obesity prevalence of 40%,17,18 which exceeds state and national levels.1 Participants were child-parent dyads. Children (ages 7 to 12 years old) were over- weight or obese (BMI ≥85th for age and sex). We previously reported that our participants had high cardiometabolic risk.19 Recruitment and enrollment occurred from July 2009 through December 2011. Inclusion/exclusion criteria have been published elsewhere.19,20 One parent (or primary caregiver) per child were enrolled in the study. Two to 3 visits were used to obtain baseline data. Families could begin completing questionnaires after providing consent/ assess, complete additional questionnaires during pre-randomization visit for obtaining fasting blood specimens, and could finish completing question- naires during a third visit in which eligibility was verified prior to randomization.
Independent survey data were not available for siblings, limiting this study to 301 parent-child (in- dex) dyads that had complete anthropometric and survey measurements assessed in our analyses. As previously described,14 536 children were assessed for eligibility, of which 170 were excluded for the following reasons, which were not mutually exclu- sive; overall, 23 did not meet inclusion criteria, 80 declined to participate, and 76 did not complete baseline assessments. A total of 360 eligible children assented. In the case that the child recruited into the study (called the index child) had sibling(s) that met eligibility criteria, the sibling(s) was invited to participate (N = 42); however, surveys used in this analyses were for the index child only.
Home Environment Factors and Health Behaviors of Low-income, Overweight, and Obese Youth
422
Dependent Variables Children’s dietary intake. Children’s fruit, veg-
etable, and sugar-sweetened beverage (SSB) intake, defined in Table 1, were assessed using the Block Kids 2004 Food Frequency Questionnaire (Block Kids FFQ) Spanish version (NutritionQuest, Berkeley, CA). The Spanish version contains food items of typical Mexican-Americans diets that were selected using nationally representative surveys.21 The Block Kids FFQ is a widely accepted reliable instrument22 with a third-grade reading level. It has been validated for use among racial/ethnic minor- ity children ages 8 to 17 years of age.23 In addition, it is a valid estimate of beverage intake among chil- dren ages 7 to 9 years,24 and has been used to mea- sure sugar-sweetened beverage intake in children as young as 3 to 5 years old.28
The Block Kids FFQ,25 available in English or Spanish languages, was obtained during an in- person interview at baseline conducted by trained, bilingual (English/Spanish) research staff with chil- dren and parental assistance, as needed for clari- fication. The Block Kids FFQ25 Spanish version consists of 84 food/beverage line items and takes approximately 25 minutes to complete. Instruc- tions on the Block Kids FFQ asked children (and assisting parents), “How many days last week?” did they eat a specific food item(s), and to include foods eaten at home, at school, from fast food, or from a restaurant. Responses were recorded using a 6-point frequency of intake scale: none, 1 day, 2 days, 3–4 days, 5–6 days, or every day. Portion sizes for each item were determined using a hand- out with pictures of serving sizes to enhance the accuracy of quantification.
Block Kids FFQs25 were mailed to Nutrition- Quest (Berkeley, CA) for data processing and anal- yses. Data output provided daily average intake of food groups based upon the USDA MyPyramid Equivalents Database (MPED) version 2.0.26 Table 1 provides definitions of children’s dietary intake measures and selected cut-points for data coding in bivariate and logistic regression analyses. We assessed fruit and vegetable intake, respectively, in cup equivalents, which is consistent with the 2015 Dietary Guidelines for Americans (DGAs).27 Both fruit and vegetable intake were dichotomized for analyses as < 1 cup equivalent per 1000 kcal/ day versus ≥ 1 cup equivalent per 1000 kcal/day,
based on the 2015 DGAs27 intake recommenda- tions for children. We assessed SSB intake by the total number of kilocalories (kcal) per day from SSB, calculated as (kcal/day from SSB)/(total kcal/ day). This method adjusts for differences in total energy intake to facilitate comparisons across sex and age groups, and has been used to estimate na- tional trends in SSB intake.28 SSB intake was di- chotomized for analyses as < 5% kcal/day versus ≥ 5% kcal/day. This cut-point was selected based on DGA27 recommendations to limit added sugar and solids fats be to 5%-15% of total daily calories.27 Most added sugars in the US diet are from sugar- sweetened beverages (soda, energy drinks, sports drinks, and fruit drinks).28 Children who did not complete the Block Kids FFQ (N = 8) and children with implausible reported energy intakes of ≤ 500 kcal/day were excluded (N = 16) from analyses, limiting the sample size for diet-related outcomes to 277 parent-child dyads.
Children’s physical activity. Children’s seden- tary time and moderate-vigorous physical activity (MVPA) were objectively measured using the Acti- graph GT3X accelerometer (ActiGraph, Pensacola, FL). Accelerometers are activity monitors that cap- ture the intensity of an individual’s daily physical activities in units of measurement called counts. ActiGraph accelerometers have established validity for use among children ages 6 to 16 years old.29-32
According to standardized procedures,33 chil- dren were instructed to wear the accelerometer on their hips at waistline for 5 days, excluding during bedtime, bathing, and swimming. To be included in this analysis, children must have had 10 hours of valid wear time for 3 or more of the 5 days. Non-wear periods were defined as 60 minutes of consecutive zero counts with an allowance for up to 2 minutes of nonzero counts.34,35 Data from the accelerometer were downloaded, processed and screened for wear time.
Epoch lengths (sampling intervals) of 60 seconds were used to determine activity cut-point values.36 The GT3X device has an inbuilt inclinometer that detects standing, lying, sitting and “off.” The Ac- tiGraph algorithm classifies counts >100 counts min−1 as standing. If the counts are below 100, the data from the axes is used to classify sitting or lying or “off.” Thus, this analysis defined sedentary time as <100 counts min−1.
Colon et al
Am J Health Behav. 2019;43(2):420-436 423 DOI: https://doi.org/10.5993/AJHB.43.2.17
2019;43(2):420-436 423 DOI: https://doi.org/10.5993/AJHB.43.2.17
Whereas several definitions of sedentary time have been proposed, there is no standard definition of the term. It is recommended to use cut-points that are consistent with unit of analysis (eg, epoch length), instrumentation.37 Our analysis defined sedentary time using < 100 counts min−1 because threshold has been calibrated30 and validated29,38 to measure sedentary time and physical activity with the ActiGraph accelerometer in young children (ages ≥ 3 years old), and is consistent with pub- lished literature using the ActiGraph GT3X.19,34
A MET is an estimate of relative intensity such that 1 MET represents the energy expenditure for an individual at rest; whereas a 5 MET activ- ity requires 5 times that amount. Average time (minutes/day) spent in MVPA was calculated by using an age- and sex- specific energy expenditure prediction equation, developed by Freedson et al39 and used by others31,33,40 for count cut-points that correspond to levels of PA measured in metabolic equivalents (METS): 2.757 + [0.00153 x counts/ minute] – [0.0896 x age (years)] – [0.000038 x counts/minute x age (years)]. Table 1 provides defi- nitions of children’s sedentary time and MVPA, and selected cut-points for data coding in bivariate and logistic regression analyses. Sedentary time was di- chotomized for analyses as < 8 hours/day versus ≥ 8 hours/day, based on the average time that American youth spend engaged in sedentary time, which in- cludes hours during and outside of school. Specific recommendations for total time spent in sedentary time are not available.41,42 MVPA was dichoto- mized for analyses as < 60 minutes/day versus ≥ 60 minutes/day, based on the DGAs27 and American Academy of Pediatric recommendations4,41,42 for children to perform 60 minutes or more of physi- cal activity per day, of which most of the minutes should be either moderate- or vigorous-intensity.
The biggest barrier to accelerometer data collec- tion was children forgetting to put on the acceler- ometer, resulting in non-wear periods. We excluded 88 (29.2%) children from this analysis due to too few (< 3) valid accelerometer wear days. Compared to children with ≥ 3 valid wear days (data not shown), these children had a greater proportion of parents that obtained more than a high school education (34.1% vs 23.0%; p = .05). No other statistically significant differences in child/parent characteristics, HE, or anthropometric measures
assessed in this study were observed between the 2 groups. This limited the sample size when sed- entary time or MVPA were dependent variables to 213 parent-child dyads.
Independent Variables Sociodemographic and home environment sur-
veys (available in English and Spanish) were admin- istered face-to-face by trained, bilingual (English/ Spanish) research staff. Parental and child sociode- mographic and home environment questionnaires were answered by the parent. Additional details of the HE measures assessed in this analysis have been published elsewhere.20
Anthropometric. Parents’ and children’s standing heights and weights were objectively measured by trained research staff in a private patient examina- tion room using a stadiometer and digital scale, following standardized procedures.43,44 Participants wore light clothing without shoes and emptied their pockets. For children, BMI percentiles and z-scores were calculated using the SAS Program for the 2000 CDC Growth Charts (ages 0 to < 20 years),45 and categorized as overweight (BMI 85th to 94.9th % for age and sex) or obese (≥95th % for age and sex). Parents’ BMI was calculated using the formula BMI = (Weight, kilograms)/(Height, me- ters2) and categorized as normal/overweight (BMI 18.5 < BMI < 30 ) or obese (BMI ≥ 30.0).46 One parent was underweight (BMI = 16.9) and catego- rized as normal/overweight for analyses.
Sociodemographics. Due to a large proportion of Hispanics/Latino children (74.8%) in our popu- lation, race and ethnicity were collapsed: Hispanic/ Latino, Non-Hispanic black, and other. Child characteristics included age, sex, BMI percentile, weight category, and race/ethnicity. Familial char- acteristics included parent age, sex, BMI, weight category, and proportion of years spent living in the US (calculated as [(years living in the US)/ (age in years]).47 Additional sociodemographic de- tails of the study population have been published elsewhere.20
Parenting practices. The Parenting Practices for Eating and Activity Scale (PEAS) is a 26-item instrument that was developed and validated by Larios et al48,49 among Latina/Mexican-American mothers of elementary-aged children to assess par- enting strategies related to children’s dietary and
Home Environment Factors and Health Behaviors of Low-income, Overweight, and Obese Youth
424
Ta bl
e 1
D efi
ni ti
on s a
nd S
el ec
te d
C ut
-p oi
nt s o
f C hi
ld re
n’ s D
ie t a
nd P
hy si
ca l A
ct iv
it y
B eh
av io
rs (D
ep en
de nt
V ar
ia bl
es )
A ss
es se
d in
B iv
ar ia
te a
nd L
og is
ti c
R eg
re ss
io n
A na
ly se
s C
hi ld
re n’
s W
ei gh
t- re
la te
d B
eh av
io rs
(D
ep en
de nt
Va
ri ab
le s)
In st
ru m
en t
U ni
t o f A
na ly
si s
Se le
ct ed
C
ut -p
oi nt
fo r
A na
ly se
s D
efi ni
tio n
U se
d in
O ur
S tu
dy S
am pl
e
Fr ui
t I nt
ak e
B lo
ck 2
00 4
Fo od
F re
qu en
cy
Q ue
st io
nn ai
re , S
pa ni
sh V
er si
on
(N ut
rit io
nQ ue
st ; B
er ke
le y,
C A
)
C up
e qu
iv al
en ts
p er
1 00
0 kc
al p
er
da y
(U SD
A M
yP yr
am id
E qu
iv al
en ts
D
at ab
as e
ve rs
io n
2. 0)
< 1
cu p
eq ui
va le
nt p
er
10 00
k ca
l/d ay
v er
su s
≥ 1
cu p
eq ui
va le
nt p
er
10 00
k ca
l/d ay
B an
an as
; a pp
le s o
r p ea
rs ; o
ra ng
es o
r t an
ge rin
es (e
xc lu
de s j
ui ce
s) ; s
tra w
be rr
ie s o
r o th
er b
er rie
s; a
pp le
sa uc
e,
fr ui
t c oc
kt ai
l o r p
in ea
pp le
sl ic
es ; j
el ly
o r j
am ; a
ny o
th er
fr ui
t l ik
e gr
ap es
, p ea
ch es
, w at
er m
el on
, c an
ta lo
up e,
or
fr ui
t r ol
l-u ps
; r ea
l o ra
ng e
ju ic
e (e
xc lu
de s S
un ki
st o
r o th
er o
ra ng
e so
da s)
; a ny
o th
er re
al fr
ui t j
ui ce
s l ik
e ap
pl e
ju ic
e or
g ra
pe ju
ic e
(in cl
ud es
ju ic
e bo
xe s)
, a dd
iti on
al m
ix ed
fo od
sa
Ve ge
ta bl
e In
ta ke
B lo
ck 2
00 4
Fo od
F re
qu en
cy
Q ue
st io
nn ai
re , S
pa ni
sh V
er si
on
(N ut
rit io
nQ ue
st ; B
er ke
le y,
C A
)
C up
e qu
iv al
en ts
p er
1 00
0 kc
al p
er
da y
(U SD
A M
yP yr
am id
E qu
iv al
en ts
D
at ab
as e
ve rs
io n
2. 0)
a
< 1
cu p
eq ui
va le
nt p
er
10 00
k ca
l/d ay
v er
su s
≥ 1
cu p
eq ui
va le
nt p
er
10 00
k ca
l/d ay
Sa la
d w
ith le
ttu ce
, g re
en sa
la d;
a vo
ca do
, g ua
ca m
ol e;
g re
en b
ea ns
, s tri
ng b
ea ns
, o r p
ea s;
p in
to , c
hi li
w ith
be
an s,
or b
ea n
bu rr
ito ; r
ef rie
d be
an s;
sp ag
he tti
, r av
io li,
o r l
as ag
na w
ith to
m at
o sa
uc e;
v eg
et ab
le so
up ,
ve ge
ta bl
e be
ef so
up , o
r t om
at o
so up
; a ny
o th
er so
up o
r s te
w ; g
re en
s l ik
e co
lla rd
s, m
us ta
rd g
re en
s o r
sp in
ac h;
b ro
cc ol
i; ca
rr ot
s, ca
rr ot
st ic
ks , o
r c oo
ke d
ca rr
ot s;
F re
nc h
fr ie
s, Ta
te r T
ot s,
ha sh
b ro
w ns
o r h
om e
fr ie
s; a
ny o
th er
k in
d of
p ot
at oe
s, lik
e m
as he
d, b
ak ed
, o r b
oi le
d; sw
ee t p
ot at
oe s,
sw ee
t p ot
at o,
o r p
um pk
in
pi e;
a ny
o th
er v
eg et
ab le
s l ik
e sq
ua sh
, c au
lifl ow
er , a
sp ar
ag us
, n op
al es
; k et
ch up
, s al
sa , o
r b ar
be cu
e sa
uc e,
ad
di tio
na l m
ix ed
fo od
sb Sp
an is
h ad
de d
fo od
s: ta
m al
es o
r t am
al e
pi e;
c oo
ke d
gr ee
n ch
ile p
ep pe
rs ; c
oo ke
d gr
ee n
pe pp
er s,
ch ile
re
lle no
s, or
g re
en c
hi le
st ew
; o th
er st
ar ch
y ve
ge ta
bl es
li ke
y uc
ca o
r p la
nt ai
ns
Su ga
r- sw
ee te
ne d
B ev
er ag
e (S
SB )
In ta
ke
B lo
ck 2
00 4
Fo od
F re
qu en
cy
Q ue
st io
nn ai
re , S
pa ni
sh V
er si
on
(N ut
rit io
nQ ue
st ; B
er ke
le y,
C A
)
Pe rc
en ta
ge o
f t ot
al e
ne rg
y in
ta ke
, kc
al /d
ay , f
ro m
S SB
c
SS B
in ta
ke <
5 %
k ca
l/ da
y ve
rs us
≥ 5
% k
ca l/
da y
So da
s l ik
e C
ok e,
D r.
Pe pp
er , 7
-U p,
S pr
ite , S
un ki
st , O
ra ng
e C
ru sh
(e xc
lu de
s d ie
t); sl
ur pe
es , s
no w
c on
es ,
po ps
ic le
s ( no
t i ce
c re
am );
H aw
ai ia
n Pu
nc h
, K oo
l-A id
 , S
, S
un ny
D el
ig ht
 , G
, G
at or
ad e
, i ce
d te
a,
Sn ap
pl e
; H i-C
 , T
, T
an g,
T am
pi co
 , M
, M
r. Ju
ic y
, S si
ps p
un ch

Se de
nt ar
y Ti
m e
A ct
ig ra
ph G
T3 X
A cc
el er
om et
er
(P en
sa co
la , F
L)
m in
ut es
/d ay
< 8
ho ur
s/ da
y ve
rs us
≥
8 ho
ur s/
da y
Th e
am ou
nt o
f t im
e sp
en t i
n pe
rio ds
o f a
ct iv
ity w
ith c
ou nt
s t ha
t c or
re sp
on de
d to
< 1.
The post Childhood obesity is a major health concern in the United States (US) with significant disparities among racial/ethnic minority subgroups1 and children with lower socioeconomic status.2 National Health and Nutrition Examina- tion Survey data from 2013-2014 indicate that the prevalence of obesity is higher and occurs at a younger age among black and Hispanic youth with appeared first on Infinite Essays.
"If this is not the paper you were searching for, you can order your 100% plagiarism free, professional written paper now!"