Doctors use urinary catheters to empty urine from patients who have impaired urinary system. Such patients might suffer from kidney failure due to pressure exerted on their kidneys, this is dangerous and can permanently damage their kidneys.
Doctors use urinary catheters to empty urine from patients who have impaired urinary system. Such patients might suffer from kidney failure due to pressure exerted on their kidneys, this is dangerous and can permanently damage their kidneys..
Running head: PICOT AND LITERATURE SEARCH 1
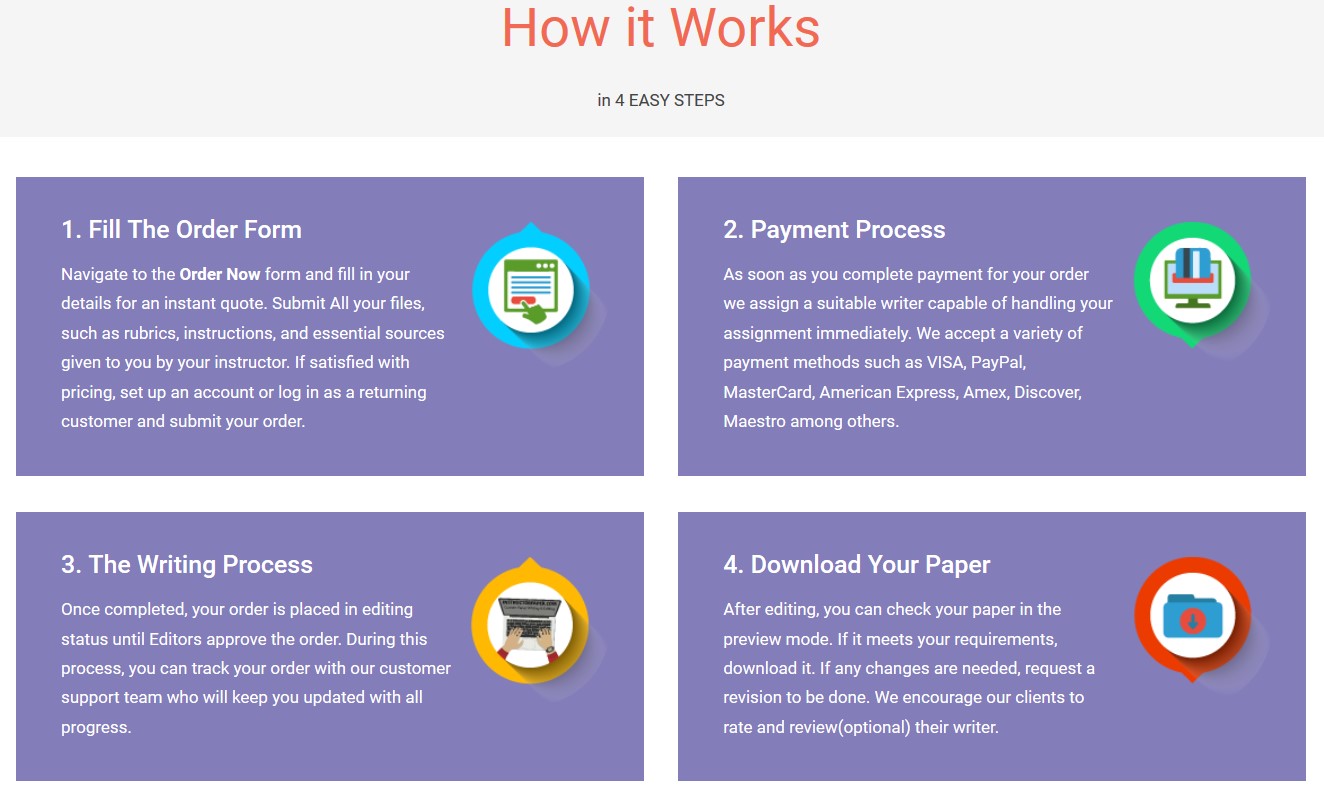
Save your time - order a paper!
Get your paper written from scratch within the tight deadline. Our service is a reliable solution to all your troubles. Place an order on any task and we will take care of it. You won’t have to worry about the quality and deadlines
Order Paper Now
PICOT and Statement Literature Search
Student’s Name: Yeni Hernandez
Date: 7/22/2018
Course: NRS-433V
PICOT and Statement Literature Search
Nursing Practice Problem
Doctors use urinary catheters to empty urine from patients who have impaired urinary system. Such patients might suffer from kidney failure due to pressure exerted on their kidneys, this is dangerous and can permanently damage their kidneys. The Urinary catheters, however, may cause potential complications on the patients. Research carried on BMC Urology shows that most patients end up suffering from urinary tract infections (UTI) after the use of indwelling urinary catheters. Other complications such as kidney damage, injury to the urethra, bladder stones, and blood in the urine, septicemia and allergic reactions may arise from the usage of the urinary catheter (Feneley, Hopley, & Wells., 2015).
Picot Statement
Prognosis/Prediction: For pediatric patients 65 years and older (P), how does the use of catheters for much longer time (I) compared to the use of indwelling catheters for shorter time(C) influence the risk of Catheter-associated urinary infections(O) during the first ten weeks of indwelling catheter usage(T)?
Most patients who are placed in indwelling catheters for more than the expected time have had the risk of developing urinary tract infections, allergic reactions and others experience challenges in their kidneys.
What are some of the practical methods used to ensure that catheter-related diseases are reduced?
This study aims to make sure that indwelling urethral catheters (IDC) are carried out in a manner that minimizes risks to infection and trauma (Conway & Larson, 2011).
1st study
Feneley, R. C., Hopley, I. B., & Wells, P. N. (2015). Urinary catheters: history, current status, adverse events and research agenda. Journal of Medical Engineering & Technology, 39(8), 459-470. doi:10.3109/03091902.2015.1085600
I chose this study because the there is a qualitative analysis of the article and the scale of the burden of urinary incontinence. Statistical data collected from the year 2006 to 2007 recorded millions of people in England with consistent problems, and in the year 2011, the number of patients had increased than the previous year. Studies show urinary infections have wider effects on the older generation, and those over 85 years of age suffered most, followed by those with over 65 years of age. Challenges emerge while an attempt is made to care for the old people and patients affected.
One study reveals that US nursing homes that received 420 admissions had 39% of patients experiencing a daytime urinary inconsistency most of them aged 65 years and above (Feneley, Hopley, & Wells., 2015).Clinicians often choose Catheterization as the last option due to high chances of urinary tract infections. In 2002, US had incidences of advance events of catheter induced_ infections occurring and causing deaths of about 13089 patients. Infections related to usage of catheter machine have ever raised a controversial issue regarding the development of antimicrobial resistance and distress both to the clinicians and the sufferers.
2nd study
Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nature Reviews Microbiology, 13(5), 269-284. doi:10.1038/nrmicro3432
I chose this study because the article gives a qualitative analysis of the pathogenesis of the urinary infections during catheterization. There are endogenous sources of microorganisms causing CAUTI. It originates from contaminated hands of the healthcare personnel, vaginal colonization, and meatal, contaminated equipment and rectal. These pathogens pass either through the extraluminal route, intraluminal route, through the catheter from the contaminated collected bag or travel along the outside of the catheter in the form of a periurethral mucous sheath. Introduction of the sterile objects has shown a reduction in risk of bacteriuria in a closed urinary drainage. However, studies have shown that bacteriuria can occur via breaks in the machines or through the extraluminal route. Eventually, there is a 10% daily risk of bacteriuria with catheterization and about 100%risk in a month; this occurs in a short and long-term duration of catheterization (Flores-Mireles, Walker, Caparon & Hultgren, 2015). If clinicians prolonged catheterization then there is a high chance that the urinary pathogens would form biofilms on the surface of the catheter. With time, the microorganism begins to colonize on the surface of the urinary catheter in an immobile state. Hence it becomes resistible to antimicrobials, and their eradication becomes impossible without removal of the catheter.
3rd study
P., J. (2013). Urinary incontinence and the importance of catheter fixation. Journal of Community Nursing, 27(5), 24-29. Retrieved from http://www.southernhealth.nhs.uk/_resources/assets/inline/full/0/70589.pdf
I chose this study because the article qualitatively highlights the process for insertion of the urinary catheter. The guidelines recommend that a trained and a competent doctor should carry the process of IDC insertion in urinary catheterization. It is also imperative that the specialist should conduct the following Aseptic technique procedures depending on gender patients. For female patients, a doctor would have to perform hand hygiene, place a patient in a supine pose with hips flexed and knees bent. In case of soiling evidence, a clinician should clean the genital area with water and soap before conducting the primary procedure. Hand hygiene is necessary at this point after which the Doctor would open the dressing pack in an aseptic field and prepare the needed equipment using aseptic technique. To avoid contamination saline is sterilized and poured onto a tray and hand wash is done under aseptic environment, a doctor should also wear sterile gloves apply sterile towel and separate labia with one hand to expose the urethral opening. Using swabs apprehended in forceps with another hand a specialist would clean the labial folds, and the urethral opening then moves the swab from above urethral opening downwards towards the rectum (J., 2013).After each urethral fondle, a doctor should discard swab into a designated waste bag and remove the catheter wire. Following the procedural guidelines, the doctor would then lubricate the catheter, insert it into urethral opening upward at about 30 degrees until urine begins to flow. The doctor should inflate the balloon slowly in the last procedure using sterile water and check if the patient feels any pain, if not then they would deflate the balloon and insert the catheter further and ensure that urine is flowing before inflating the balloon again (J., 2013).
4th Study
Lee, N. G., Marchalik, D., Lipsky, A., Rushton, H. G., Pohl, H. G., & Song, X. (2016). Risk factors for catheter-associated urinary tract infections in a pediatric institution. The Journal of Urology, 195(4), 1306-1311. doi:10.1016/j.juro.2015.03.121
I chose this study because the article qualitatively describes the effects of using the catheter on patients with urinary complications. Half of the patients placed in catheterization for more than seven days have a high chance of contracting bacteriuria. Health care workers perform an intervention on the urinary system either to empty the bladder, facilitate the installation of a solution or medication or to dilate a urethral stricture through the insertion of the catheter. When performing clinical care, the inclusion of the catheter on the patients may lead to catheter-associated urinary tract infection (CAUTI) depending on the host susceptibility, quality of catheter care duration, method of catheterization. If the catheter specialist fails to follow guidelines and leave the catheters for a longer period, then the infections may arise and traumatized the urinary tract (Lee, et al., 2016).
5th Study
Meddings, J., Rogers, M. A., Krein, S. L., Fakih, M. G., Olmsted, R. N., & Saint, S. (2014). Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Quality & Safety, 23(4), 277-289. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3960353/
I chose this study because the guideline gives qualitative highlights of some of the proper measures that a doctor should undertake while performing a catheterization. When conducting insertion of the urinary catheter, a trained doctor should take special precautions since rapid drainage of urine from the bladder may cause hemorrhage. A clamp should also be released after every 20 minutes to allow more drainage of urine. A clinician is required to use electrolyte after post-obstructive diuresis IV replacement under the discussion of treating medical team. Based on an ongoing nursing management a doctor should measure and access urine output after every 1-4 hour, in case of any variation in the usual amount of urine which is usually 1-2ml/kg/hr., then a doctor should report the matter to the medical team (Meddings, et al., 2014).The doctor should adhere to sterilization throughout the process, and avoid any breaches to the closed system; this reduces the risk of catheter-associated infections. The Guidelines on nursing management recommends that a doctor should position drainage bag to prevent backflow of urine and change the catheter tube to prevent obstructions of the disconnected system, contamination, and infections. For proper hygiene, carers should maintain routine cleanliness by ensuring they shower patients and clean the IDC insertion site with warm water and soap. Moreover, the doctor should consider removing the IDC when it is no longer in need to lessen the risk of urinary tract infection (UTI).
Proposed Evidence-Based Practice Change
Conway, L. J., & Larson, E. L. (2012). Guidelines to prevent catheter-associated urinary tract infection: 1980 to 2010. Heart & Lung: The Journal of Acute and Critical Care, 41(3), 271-283. doi:10.1016/j.hrtlng.2011.08.001
I chose this study because the Clinicians in this article used Qualitative analysis of to examine patients in ICU who are under the care of catherization. Additionally, this study supports the premise of the paper by providing a solution to the problem in the PICOT question. The specialist catheterizes only those in need of catheterization to avoid damages on the urinary tract system. Also, performers carried the process of catheterization using aseptic techniques, and they ensured that sterilization of the equipment was strictly adhered to; also they used closed and sterile drainage system throughout the treatment session. The doctors examine the patients under the care of indwelling catheter at an interval of 4 weeks and ten weeks. Results revealed that some pediatric patients who were under the care of indwelling catheters for more than six weeks were beginning to develop the catheter-associated urinary infection while those placed in catherization for less than four weeks were still healthier. This is an indication that timing of catheter change should be a priority throughout the process, nurses should treat each differently because other patients have a greater risk of developing Catheter-related diseases. To minimize the risk of urinary infections and other related infections doctors should change the indwelling catheters after two weeks or three weeks depending on different individuals. The guidelines on this article recommend all persons to be responsible during the insertion of the catheters and that clinicians should have to go through a thorough training, the nurses in this study documented the analysis of catherization as per the guidelines (Conway & Larson, 2011).Above all the doctors provided a feedback information regarding the clinical measures to administrators.
Conclusion
National quality and regulatory initiatives are aligned together with the guidelines for preventing CAUTI. Prioritizing the cleanliness and maintaining an aseptic environment is a key factor that clinicians should worry. Also the clinicians should ensure that closed urinary drainage system is maintained to meet a regulatory and a quality requirement in the hospital.
References
Conway, L. J., & Larson, E. L. (2012). Guidelines to prevent catheter-associated urinary tract infection: 1980 to 2010. Heart & Lung: The Journal of Acute and Critical Care, 41(3), 271-283. doi:10.1016/j.hrtlng.2011.08.001
Feneley, R. C., Hopley, I. B., & Wells, P. N. (2015). Urinary catheters: history, current status, adverse events and research agenda. Journal of Medical Engineering & Technology, 39(8), 459-470. doi:10.3109/03091902.2015.1085600
Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nature Reviews Microbiology, 13(5), 269-284. doi:10.1038/nrmicro3432
Lee, N. G., Marchalik, D., Lipsky, A., Rushton, H. G., Pohl, H. G., & Song, X. (2016). Risk factors for catheter-associated urinary tract infections in a pediatric institution. The Journal of Urology, 195(4), 1306-1311. doi:10.1016/j.juro.2015.03.121
Meddings, J., Rogers, M. A., Krein, S. L., Fakih, M. G., Olmsted, R. N., & Saint, S. (2014). Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Quality & Safety, 23(4), 277-289. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3960353/
P, J. (2013). Urinary incontinence and the importance of catheter fixation. Journal of Community Nursing, 27(5), 24-29. Retrieved from http://www.southernhealth.nhs.uk/_resources/assets/inline/full/0/70589.pdf
The post Doctors use urinary catheters to empty urine from patients who have impaired urinary system. Such patients might suffer from kidney failure due to pressure exerted on their kidneys, this is dangerous and can permanently damage their kidneys. appeared first on Infinite Essays.
"If this is not the paper you were searching for, you can order your 100% plagiarism free, professional written paper now!"