Soap Hypertension and Depressive Disorder
APA stile, no plagiarism. This is an example of SOAP notes:
Patient Information
Name: Mr. R.G.
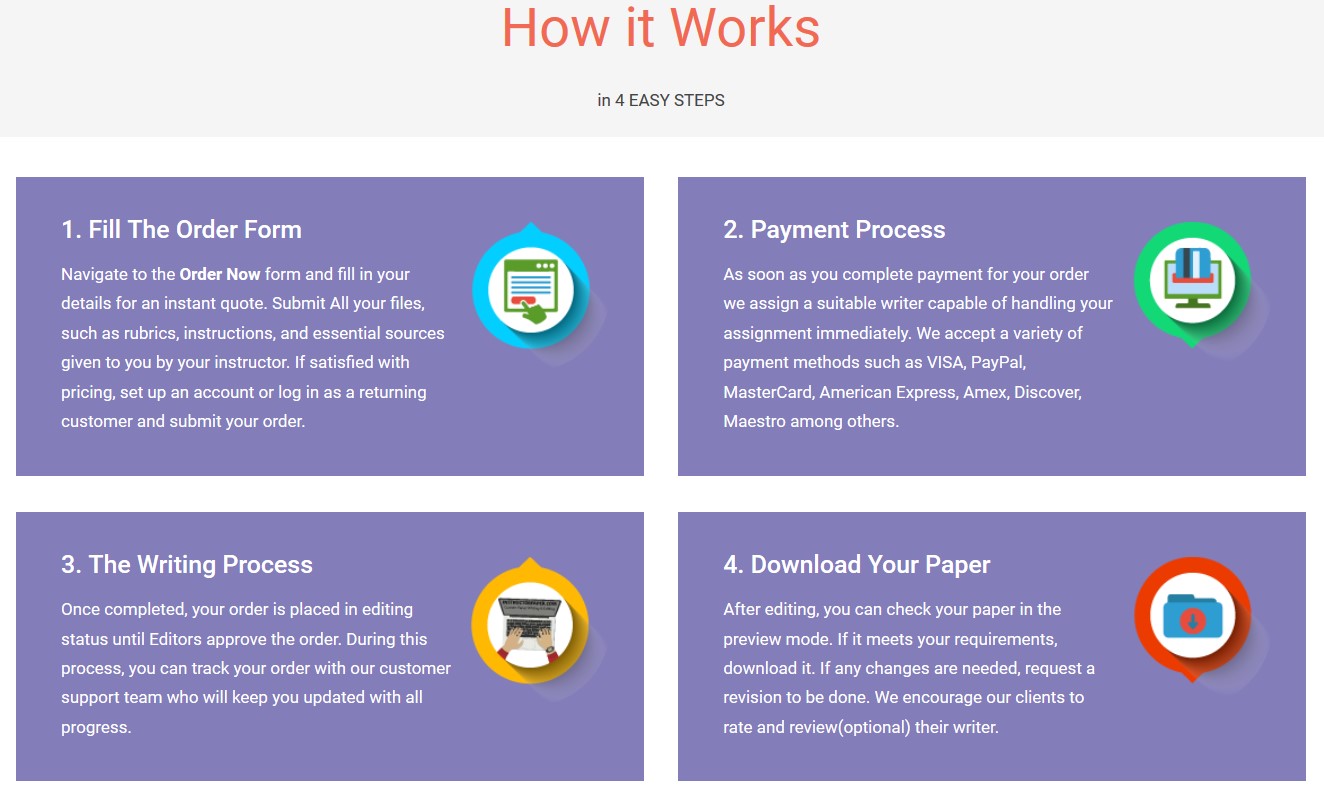
Save your time - order a paper!
Get your paper written from scratch within the tight deadline. Our service is a reliable solution to all your troubles. Place an order on any task and we will take care of it. You won’t have to worry about the quality and deadlines
Order Paper NowAge: 58-year-old
Sex: Male
Source: Patient
Allergies: No known allergies. No seasonal allergies detected
Current Medications: No current medication mentioned by the patient.
PMH: The patient has been abusing alcohol but quit two years back. He is suffering from obesity disorder and hypothyroidism.
Immunizations: Immunization is up to date.
History of the Family: Mother- deceased at 70 years, no information related to the cause of his death but was having obesity disorder.
Father still alive: History of Type II diabetes, Hypertension
Soap Notes
Subjective
Chief Complain (CC): the patient came to the facility complaining of heat intolerance, and sweating.
HPI: Mr. R.G he is having an increased nervousness, sweating, and hotness of the body.
ROS
General: Patient appears to be weak and fatigue. He has a loss in the body weight, poor sleep, thirst, nausea, and increased frequency of defection. He also states of losing appetite and shaking.
Constitutional: The patient denies of having chest pain, palpitations, shortness of breath, and disorientation.
Respiratory: No shortness of breath with no asthma or seasonal allergies
Cardiovascular: no history of Dyslipidemia, no history of high blood pressure. He has no dyspnea on exertion, there is absent of cough, edema, or heart murmurs.
Gastrointestinal: the patient has nausea but no vomiting. The patient has lost appetite.
GU: He denies vaginal discharge, no irritation in his urinary tract.
Objective
Mr. R.G appears to be little disturbed, maintains his eye contact, clearly gives a proper description of how he feels and his age, and the dressing as per the present weather.
Vital Signs: B/P: 105/95 mmHg, Regular pulse of 90 beats per min, Temprature: 96.5; Height: 70 inches; weight: 113 lb: BMI: 16.2.
Clear and normal breathing sounds with no adventitious breathing sounds. Goiter noted on palpation.
Cardiovascular: no apparent distress, fidgeting in the seat, no presence of murmurs and gallops.
Gastrointestinal: soft and non-tendered abdomen when touched.
GU: suprapubic regions are tender to touch
Assessment
Hyperthyroidism, a disease related to Graves’ illness
Plan
To acquire the baseline thyroid stimulating hormone assay; prescription of the antithyroid medications such as Carbimazole and propylthiouracil; performing thyroid hormone level using thyroid stimulating hormone blood test.; monitoring the thyroid-stimulating hormone assay at first and the third months, performing radioactive iodine treatment when necessary. In case the thyroid hormone level is not improved, thyroid lobectomy will be performed
Soap Hypertension and Depressive Disorder
"If this is not the paper you were searching for, you can order your 100% plagiarism free, professional written paper now!"